Building a Global Framework for Digital Health Services in the Era of COVID-19
Health data and digital technologies will be essential for improving health outcomes across the globe beyond the COVID-19 pandemic. Low- and middle-income nations, with fledgling digital health strategies and many barriers to overcome, stand to benefit the most.
KEY TAKEAWAYS
The Building Blocks for Digital Health
International Governance to Support the Protection, Flow, and Use of Health Data
Multilateral Governance and Support of Digital Health
Appendix: Case Studies Showing How Digital Health Can Help LMICs
Overview
Digital health—the use of information and communications technology (ICT) to provide and improve health services—holds transformational potential for health care around the world. Many digital health products are already proven, readily available, and adaptable to all kinds of countries. Digital health can help low and middle-income countries (LMICs), in particular, overcome traditional barriers to better health care, especially staffing and other physical resource constraints. Digital technologies are showing their potential during the current coronavirus crisis by facilitating collaboration between health-care researchers and reducing the need for in-person care. While health data and digital technologies are not a silver bullet to COVID-19 and other health issues, they will be crucial to improving overall health outcomes in countries around the world. LMICs need to work with international partners, such as the World Health Organization (WHO) and development banks, to marshal the resources, expertise, and strategies to help them realize the true potential of digital health.
COVID-19 underlines the importance of international cooperation and collaboration to global health.
A global digital health framework is only at a nascent stage. Understandably, policymakers in all countries are first dealing with the considerable challenge of adapting technology to their own domestic health frameworks. And international organizations are only just starting to develop the common principles, best practices, and tools to help late adaptors and developing countries catch up with leading countries. The risk is domestic frameworks will fragment away from international standards, thereby preventing health companies and research organizations from leveraging health data and digital technologies in order to provide new and better services across different countries. COVID-19 has underlined the importance of international cooperation and collaboration to global health.
LMIC policymakers and their international health and development partners must focus on foundational issues—namely, a national digital health strategy, digital skills, ICT infrastructure, and data governance—to build effective domestic and global digital health frameworks. This report aims to support these policymakers in doing this. The first section outlines the promise of digital health (the appendix includes case studies from several regions that illustrate how this is working in practice). The paper then gives an overview of core enablers for digital health, including an analysis of the importance of ICT infrastructure and digital skills, and domestic and international data governance. The paper then reviews the growing focus on digital health by multilateral organizations and other nongovernmental organizations (NGOs).
The paper concludes with general findings and recommendations, summarized below:
- Countries should develop holistic national digital health strategies. There is wide disparity in progress in this area among LMICs, with several important countries having no formal national plans. Digital technologies will not achieve anywhere near their full potential absent a plan that provides the necessary resources, coordination, cooperation, and leadership. These plans need to be holistic, in part, as each country’s situation will be somewhat different, including the considerable complexity that comes from integrating digital technologies with legacy health systems.
- Several multilateral organizations and private-sector initiatives have elevated the focus on digital health at the international level, such as the WHO-backed global digital health strategy. LMICs should work with WHO and other actors to mobilize the resources and expertise to help develop and implement—or improve—their own digital health strategies.[1]
- Training and education to use digital technologies is critical, but few LMICs have integrated digital skills into their health-workforce training. Regional and multilateral health organizations, donors, and other stakeholders should prioritize efforts to help LMICs address the most pressing skills gaps.
- There are particularly acute gaps in ICT infrastructure in LMICs, which are home to most of the people that remain disconnected from the Internet. Poor ICT infrastructure severely limits the potential of digital health. Regional and multilateral development agencies, and other donors, should fill these gaps to cover private-sector shortfalls—for example, with regard to wireless mobile coverage in rural areas.
- LMICs need to enact a data governance framework that balances data privacy and protection with innovation. The generation, protection, use, sharing, and international transfer of high-quality data is fundamental to an effective and innovative digital health program. An overly restrictive data governance framework will limit the potential of digital health technologies.
- Policymakers need to build interoperability into their frameworks from the start, as many of the benefits of digital health technologies require cross-border transfers of data. This is critical, as many firms and research organizations involved in digital health rely on the Internet, the free flow of data, and centralized IT facilities to easily, cheaply, and reliably access data, patients, and health-care providers around the world. The emergence of a meaningful, integrated global digital health framework will depend on national governments enabling cross-border flows of data.
The Promise of Digital Health
Simply put, “digital health” refers to the use of digital technologies for health. It is an umbrella term that includes electronic health (eHealth), mobile health (mHealth) and emerging areas such as the use of artificial intelligence (AI), big data, and genomics.[2] As populations age and noncommunicable disease burdens rise, there will be even greater pressure on health-care systems, underscoring the need to deploy current and new technological solutions.[3] WHO has stated that “universal health coverage cannot be achieved without the support of eHealth.”[4]
Digital health holds considerable promise.[5] It can make health information, care, and diagnosis more accessible, such as through telemedicine.[6] This is especially true for people in hard-to-reach places, given the proliferation of low-cost smart phones and medical devices. Digital health can enable health-care providers and services to become more efficient and of higher quality. In particular, the enhanced use of health data offers the prospect of more personalized and coordinated care, and better, faster treatment at a lower cost.[7] AI has advanced to the stage where it can mitigate shortages of specialists, providing reliable diagnosis and lower-cost services in fields ranging from tuberculosis to diabetic retinopathy. Similarly, AI can use the greater availability of health data to identify and prevent emerging health issues, such as epidemics. When combined with software, better, richer datasets allow health system managers to identify, plan, and allocate resources more efficiently. Digital health can also accelerate the drug development process.[8] For example, AI can integrate and analyze a broader range of “real-world” data from mobile and wearable technologies and social media, and combine it with traditional lab and clinical data.[9]
Many of these benefits are already evident, and hold particular promise for LMICs given they can be deployed at significantly lower cost than traditional brick-and-mortar health services. Indicative of this, digital health technologies are currently undergoing a surge in uptake. Globally, 44 percent of mobile users have seen a medical professional for diagnosis or treatment via their mobile device.[10] According to IQVIA (a U.S. health technology firm), the number of mHealth products and services has doubled in the past 5 years in LMICs, and there are now over 165,000 mobile applications for health services.[11] In fact, mobile health services are more popular in LMICs, with 59 percent of patients in LMICs using mHealth applications and services, compared with 35 percent in high-income countries.[12]
As populations age and noncommunicable disease burdens rise, there will be even greater pressure on health-care systems, underscoring the need to deploy current and new technological solutions.
There is potential for digital health to benefit the wider economy, not only through significant cost savings but also via increases in productivity as patients receive faster, more accurate diagnoses and treatment.[13] For example, Canada measured the cost savings generated by its digital health investments and reported an aggregate saving of US$11.2 billion since 2007.[14] Many studies anticipate considerable cost savings from digital health, such as a 2013 GSMA study that estimated mHealth technology could result in $400 billion worth of cost savings over a 5-year period in high-income countries.[15] A review of 14 evaluations of digital health interventions across a range of high-income countries found them all to be cost effective and an improvement over existing interventions.[16]
The Building Blocks for Digital Health
Despite the potential benefits of digital health, few nations have put in place the policies, programs, or strategies needed to take full advantage of it. The 2019 Global Digital Health Index assesses the state of preparedness and adoption of digital health in 22 countries of varying stages of economic development (see figure 1).[17] It also measures the readiness of the wider health system to successfully adopt and deploy digital health interventions. The Index is benchmarked according to components of the WHO and International Telecommunications Union (ITU) eHealth Strategy Framework, which uses 19 indicators in 7 policy areas: leadership and governance; strategy and investment; services and applications; standards and interoperability; infrastructure; legislation, policy and compliance; and workforce.
The Index notes that while many countries have national digital health strategies, most lack national digital health architectures, health information exchanges, and data standards, all of which undermine the potential benefits of digital technologies.[18] This section explores some of the core enablers of the Index—education and workforce training, infrastructure, and governance—in explaining what makes an effective digital health strategy.
Figure 1: 2019 Global Digital Health Index[19]
National Digital Health Strategies
Developing a national digital health strategy is a critical first step for identifying, prioritizing, and addressing barriers and shortfalls in key enablers for digital health. A comprehensive local assessment is crucial to developing a long-term plan, coordinating with development and other partners, and mobilizing the political support necessary for resourcing and implementation.[20]
An effective digital health strategy requires leadership and buy-in from federal (and regional) governments, supported by representatives from all relevant government agencies and nongovernment stakeholders, including the private sector, nonprofit organizations, and overseas development agencies. A whole-of-government approach is needed as health agencies cannot operate in a silo disconnected from ICT, economic, science, health, and innovation agencies, as well as data privacy and protection agencies.
Proper financial support is essential, especially given new programs and technologies will be layered on top of existing IT systems and organizational structures, which often means significant up-front costs. This also highlights the need for governments, development partners, and other stakeholders to invest in coordinated plans rather than ad hoc projects and policies. Unfortunately, many LMICs have already succumbed to the latter approach and face a proliferation of uncoordinated digital health projects, which is more likely to lead to unsustainable and ineffective uses of digital health tools.[21]
While many countries have recognized the importance of national digital health strategies, there are significant gaps in many regions around the world. WHO’s 2015 survey of eHealth policies revealed that 72 countries (58 percent) of the 125 member countries (that responded) have defined national digital health strategies and corresponding plans to implement them (see figure 2).[22] Notable exceptions include Brazil, India, Indonesia, and Mexico. The Global Digital Health Index observes that Malaysia, the Philippines, and Jordan are well advanced in this area, with fully costed national plans currently being implemented.[23] Malaysia in particular is lauded for its integrated digital health strategy, which has been ongoing for 15 years and is linked to the national 5-year rolling Malaysia Plans for social and economic transformation.
Thankfully, international agencies are working to help countries that have yet to develop a national strategy. For example, WHO’s International Telecommunications Union (ITU) National E-Health Strategy Toolkit aims to assist member states in the development and implementation of digital health policies and strategies, and subsequent integration with their national health-care systems. The toolkit is an expert, practical guide that provides a solid foundation and method for developing and implementing a national digital health vision, action plan, and monitoring framework.
Figure 2: Countries with national eHealth policies or strategies[24]
People Need the Right Skills to Leverage Digital Health
Using data and digital technologies for better health outcomes is contingent on a nation having a digitally competent workforce. The lack of digital skills is obviously not unique to the health-care sector in LMICs, but given the impact on people’s well-being, requires special attention. Skills shortages directly undermine the use of digital health interventions.[25]
Unsurprisingly, in many LMICs, there are basic digital skills shortages across both the health workforce and patients, especially in rural and remote areas. According to the 2019 Global Digital Health Index, the skills base among health-care professionals is generally low. Only 2 of the 22 countries surveyed by the Index include digital health in training for health-care professionals, with less-significant gaps among physicians, and more-significant gaps in training for nurses and community health workers. Skills gaps are particularly pronounced in WHO’s Eastern Mediterranean region, with Southeast Asia having the strongest base of skills to enable digital health.[26]
The need to improve digital skills is recognized as a key objective of WHO’s “Global Strategy on Digital Health 2020–2024.”[27] The ideal long-term solution would be introducing or bolstering digital skills at primary, secondary, and tertiary education levels. However, given resource constraints and the need for quicker results, upskilling health workforces to make them digitally competent could be a more pragmatic strategy. Best practice involves introducing digital skills into the heath education curricula for health-care workers both pre- and post-deployment, ideally for both clinical staff and community workers. This can be done as part of general capacity building efforts as well as those related to specific digital health projects, and could happen at workforce training institutions (such as for vocational training) and private-sector-led programs (such as for re-skilling). These private-sector-led training and certification schemes could bridge the digital skills gap, without people needing to go back for formal, secondary, or tertiary-type education and training.[28]
In the longer term, governments need to find a pathway for workers to pursue STEM (science, technology, engineering, and mathematics) courses and advanced digital skills. Similarly, policymakers need to ensure people in health-policy leadership positions have the skills and knowledge to develop and manage in-country digital health initiatives and strategies.[29] An example of this is the Digital Health Leadership Program, which supports African digital health leaders, particularly those in government agencies.[30]
Ghana: Digital Skills for Pharmacists to Manage Hypertension
The community-based hypertension improvement project (ComHIP), in the Eastern Region of Ghana, offers training to licensed medicine sellers in the community to screen for and provide adequate health education and information on hypertension to their clients. This model, underpinned by a comprehensive digital health platform, maximizes opportunities for screening and diagnosis of hypertension in a peri-urban area of sub-Saharan Africa, and brings chronic disease care closer to the community. The project demonstrates how targeted training of end users of digital health platforms can be effective in improving health outcomes.
Addressing the digital skills gap for health outcomes is a major challenge made more difficult by constantly evolving technology. In late 2018, the Digital Frontiers Institute convened a seminar series entitled “Digital Health: Building a Future Proof Workforce” to examine this issue, including skills needs and gaps.[31] Some of the key gaps identified include digital health leaders, managers, and policymakers; digital health program designers and implementers; architects, programmers, engineers, and data scientists; and digital health skills for health professionals including doctors, nurses, and administrators. This highlights the challenge of ensuring countries have enough personnel with the sufficient technical expertise for back-end IT system design and operations. For example, for sustainable digital health infrastructure, participants at the Digital Frontiers Institute identified the skills required to deploy and maintain hardware, software, and connectivity, as well as the ability to build basic, reusable infrastructure that generates economies of scale.[32] Specific skills that help health systems become more adaptable to changing technology include data scientists; visualization analysts; enterprise architects; data architects and modelers; machine learning and natural language processing specialists; systems networking and communications experts, including human to machine interaction; and security and cryptography experts.
The lack of digital skills is obviously not unique to the health-care sector in LMICs, but given the impact on people’s well-being, requires special attention.
WHO’s Action Plan for the Global Strategy of Digital Health 2020–2024 proposes all WHO member states commit to enhancing training capacity, including bolstering the capacity of tertiary institutions and developing relevant curricula.[33] Encouragingly, the 2019 Global Digital Health Index reports momentum toward the creation of digital health, health informatics, health information systems, and biomedical informatics degree programs, which are starting to show promising results in creating specialized digital health workers, particularly in countries such as Bangladesh, Chile, Ethiopia, Kuwait, Malaysia, Peru, Portugal, Sri Lanka, Thailand, and Uganda. However, most countries report there is not enough training to meet current demand, and digital considerations are yet to be properly reflected in the career paths of civil servants working on health issues.
Governments, donors, and other stakeholders should develop common templates for identifying and responding to the most-needed skills, and matching them with a corresponding list of best practices and programs for training and educating workers. They could be based on a “lowest common skillset” so LMICs could work to address and get over the most critical digital skills gaps. There should be many shared factors between LMICs, meaning a common template would be useful in avoiding wasting both time and money, with each country creating its own, detailed assessment. Within this template response, regional and multilateral health organizations and relevant donors and private-sector stakeholders should work with local governments to identify and prioritize the most-pressing areas that act as bottlenecks to improved outcomes.
ICT Infrastructure Defines the Limits of Digital Health Access and Use
Digital health, like every other digital service, relies on physical ICT infrastructure. People, businesses, and government agencies need to have access to reliable and affordable Internet services, whether they are broadband or mobile networks. LMICs and their development partners need to address this costly and complicated issue before they can even get to the issues around the digital applications that rely on the Internet. Therefore, closing the ICT infrastructure gap in developing countries will be critical to closing the digital health divide.
Digital health is growing in relevance and scale as more and more people access the Internet—at the end of 2018, the ITU estimated that over half of the world’s population was using the Internet.[34] However, there is significant variation in coverage and accessibility of mobile cellular networks, especially where they are needed most: In the world’s 47 least-developed countries, more than 80 percent of the population is still offline.[35] This directly affects the ability of countries to deliver digital health programs. Not surprisingly, according to the Global Digital Health Index (which draws on the World Economic Forum’s Network Readiness Index), the maturity of digital health infrastructure has a strong correlation with a country’s stage of development.[36] However, the Index notes that some countries are focused on addressing the gap through plans to improve infrastructure for public health facilities and offices, with Bangladesh, Jordan, and Thailand particular standouts.[37]
ICT infrastructure (along with energy) attracts two-thirds of private infrastructure financing in LMICs, in large part due to the capital intensity of the sector and the clear commercial opportunities in providing Internet connectivity.[38] But this is not the case across all LMICs. This leaves gaps where national governments and development agencies have a clearer role to step in. However, development agencies have not yet deployed much capital (or attention) to improving ICT infrastructure in LMICs as part of a holistic digital development strategy. At the moment, only a small proportion of development budgets go to helping LMICs improve their ICT infrastructure. Only 1 percent of all funding provided under what are known as “Aid for Trade” programs is currently allocated to ICT solutions. Similarly, multilateral development banks are investing just 1 percent of their total investment in ICT projects.[39]
Development agencies need to consider the specific impact that gaps in ICT connectivity have on digital health plans and programs, and come up with plans and resources to help close them. It’s unlikely private-sector financing will address all gaps in connectivity, as not all projects (such as in rural areas) will be commercially viable for private firms. National governments and development partners should work together to come up with policies and resources to help build ICT infrastructure in these areas.[40] This could include new business models that aggregate demand among public buyers who want to reach marginalized and remote people, thus helping to facilitate the development of local markets for the provision of health care and other digital services—and providing incentives to make requisite investments.[41] Given those countries and communities that remain disconnected also stand to benefit the most from digital technologies, improving their connectivity should be a top priority.
Building Health Data Governance: Collecting, Protecting, and Sharing Data for Better Health Outcomes
Data lies at the center of digital health innovations. However, health data is among the most heavily restricted forms of data (in terms of collection, use, sharing, and transferring). Health data does require specific attention as it involves sensitive personal data. Yet enacting overly severe restrictions on its use does nothing to help improve health outcomes. Policymakers in countries of all stages of development have not enacted or updated laws and regulations around health data governance such that privacy and data protection concerns are addressed while ensuring there exists a clear framework for people, firms, and governments to share and use health data (in a protected and responsible manner) to achieve its maximum potential. What this shows is that there is a disconnect between policymakers (generally) recognizing the potential of digital technologies—including for health—and how it requires changes to data governance frameworks. For example, WHO’s 2015 Atlas of eHealth Country Profiles shows only 17 percent of respondents had a strategy to govern the use of big data in the health sector.[42]
The lack of supportive health data governance frameworks around the world comes amidst an explosion in the range and volume of health data and services. The proliferation of wearable technology and other smart devices has greatly expanded the volume of patient-generated health data.[43] The ubiquity of mobile phones in LMICs has changed the situation for both health systems and individuals. Already, 1 in 10 mHealth applications have the capacity to link to a sensor or device.[44] These new technologies provide opportunities to not only generate, collect, and use large amounts of real-world data related to health outcomes—defined as observational data obtained outside the context of randomized control trials and during clinical practice—but also make the delivery of new digital health services significantly cheaper and easier for a much broader range of people.[45]
The following section analyzes key issues for health data governance: improving data collection, improving data protection, and facilitating access to health data.
Using Data to Personalize Asthma Treatment
United States-based company Propeller Health has made a GPS-enabled device that tracks data about the usage of inhalers by asthma patients. The system then integrates public information from the Centers for Disease Control and Prevention (CDC) about environmental asthma triggers so health-care providers can create personalized treatment plans.
Improving Health Data Collection
A data-driven approach to health governance can address one of a government’s biggest challenges: incomplete information.[46] Digital health programs will be of limited use if they do not have the necessary data in the first place, data coverage or data quality is poor, or they do not have systems in place to update and improve on this data. It is therefore crucial that countries, and their respective regulatory agencies and international partners, include reasonable and responsible data collection efforts to ensure data is representative, complete, and useful. The private sector can play a role in helping governments and their partners understand the health of a population, such as through public-private data sharing initiatives (explored in the next section).
National governments, and their partners, need to integrate health data collection into broader initiatives in order to improve the institutional capacity of local agencies to collect data—as well as undertake health-specific initiatives to improve data collection. The challenge facing LMIC governments’ traditional data collectors, such as national statistical offices and health agencies, is substantial, as many of these agencies lack resources and independence. Misaligned program incentives can also contribute to inaccurate data collection, among other issues.[47] However, international agencies are working to address this, including at the Partnership in Statistics for Development in the 21st Century and the Praia Group on Governance Statistics, as well as at the United Nations, the African Development Bank, and other multilateral institutions.[48]
A good example is the Health Data Collaborative (HDC), a joint effort by international agencies, governments, donors, and academia to improve health data.[49] HDC partners work alongside countries (such as Cameroon, Kenya, Malawi, and Tanzania) both to improve the availability, quality, and use of data for local decision-making and in tracking progress toward the health-related Sustainable Development Goals.[50] HDC shares a wide array of datasets, including information on routine health information systems, community data, facility surveys, measurement of quality of care, logistics management and information systems, disease surveillance, population data sources, household surveys, civil registrations, and other vital demographic statistics. HDC is developing a one-stop shop for health information system standards that will include guidelines for data collection, a standardized package of recommended indicators, data quality metrics, and other harmonized standards and survey tools.[51]
A data protection framework is a basic building block that remains missing in many countries.
Within data collection efforts, it is also important to ensure data collected is representative of the population.[52] Doing so helps address the emerging “data divide”—the social and economic inequalities that may result from a lack of collection or use of data about an individual or community.[53] For digital health innovations to be useful, individuals, firms, researchers, and governments must have access (within respective data privacy and protection regimes) to high-quality data about themselves and their communities. If certain groups have no data collected about them, new inequalities may emerge as individuals in these communities are left outside digital health programs and interventions. Specifically, policymakers can enact data collection initiatives that focus on hard to-reach populations, ensure that funding programs aimed at closing the digital divide consider the impact on data poverty, and help civic leaders in low-income areas understand the benefits of data and data-collection efforts.[54]
Enacting a Balanced Health Data Privacy and Protection Framework
Data privacy and protection are particularly important in health care given the sensitivity of personal health data and the massive growth of technology that can easily generate and share this data. According to the Identity Theft Resource Center, in 2018, there were 363 data breaches globally in medical and health-care organizations.[55] Given this, it’s understandable why many people and policymakers are rightly fearful of health data breaches and misuse. But addressing this issue requires ensuring governments and firms follow an effective data protection (and enforcement) framework.
A data protection framework is a basic building block that remains missing in many countries. According to the United Nations Conference on Trade and Development, most countries around the world (107, or 58 percent) have data privacy and protection legislation in place, including specific rules governing health information. However, this leaves a sizable proportion of countries, especially LMICs, without any framework in place.[56]
Privacy and security protections are important, as rules that are too weak can make users feel uneasy about adopting new technologies and services. Obviously, the priority for LMICs is setting this baseline level of rights and responsibilities for individuals and organizations around the collection, use, storage, and sharing of data, and the enforcement of these rules. However, beyond a baseline of protections, stronger privacy protections do not translate into more digital trust and therefore more digital adoption and use.[57]
As the Information Technology and Innovation Foundation’s (ITIF) report “Why Stronger Privacy Regulations Do Not Spur Increased Internet Use” shows, the relationship between consumer trust and the adoption and use of technology and regulations is not linear or stepwise, but an inverted U-curve.[58] In the first stage, which ITIF calls the “Unruly Rise,” light regulation can increase user adoption and use of Internet applications—although consumers may have low levels of trust because regulations do not add a sufficient baseline of protections. In the second state, the “Innovation Zone,” a reasonable baseline of protections promotes both trust and innovation, thereby ensuring high levels of user adoption and use of Internet applications. However, if policymakers create overly restrictive rules, the use of online services will likely fall or grow more slowly than it would otherwise due to a reduction in supply caused by costly and revenue-limiting regulations. The dangers of the third stage, which ITIF calls “Regulatory Hell,” is that overly strict rules actually harm consumers by creating excessive burdens on digital innovation.
Figure 3: Inverted U-curve showing relationship between regulation and technology adoption and use
Data protection and privacy frameworks should therefore strive to balance the need to protect privacy and encourage innovation. A regime being too restrictive clearly impacts the latter, as a Broadband Commission for Sustainable Development (a joint initiative by the ITU and the United Nations Education, Scientific, and Cultural Organization (UNESCO)) noted, citing how this balance is necessary to create a patient-centered and sustainable health-care system.[59] The impact (and cost) of enacting an overly restrictive data privacy framework can prevent the development and use of digital health technologies.[60] This is why appropriately robust, but balanced, data protection policies should be at the heart of a country’s health data governance framework.[61]
LMIC policymakers should put the principle of accountability at the heart of their data governance frameworks.[62] When it comes to handling data, companies doing business in a country should be responsible and held accountable under that nation’s laws and regulations, regardless of whether they are located inside or outside the country wherein the firms collect or manages data. This legal responsibility should cover both the firms’ own actions and the actions of their agents and business partners. As it relates to enforcement, policymakers should focus on holding these firms accountable, regardless of where they store, process, or transfer data. Focusing on accountability, and not where data is stored, is also crucial to building integrated, interoperable markets for health services.
The accountability principle is not new. It as a central feature of one of earliest international instruments on privacy: the Organization for Economic Cooperation and Development’s (OECD) Privacy Guidelines, originally published in 1980.[63] Many nations have made it a central part of their data privacy frameworks. For example, most U.S. firms must disclose certain data privacy practices and adhere to those requirements, even when processing data outside the country, as they remain responsible for the data regardless of where it is processed. U.S. companies mitigate these risks by stipulating requirements in relevant data-handling and processing contracts they implement with other companies. For example, foreign companies operating in the United States must comply with the privacy provisions of the Health Insurance Portability and Accountability Act (HIPAA), which regulates U.S. residents’ privacy rights for health data—even if those firms move data outside the United States.
There is no “one-size-fits-all” approach to data privacy and protection, but there are common principles and processes, such as the OECD privacy principles.
Unfortunately, some LMICs are misguidedly copying and pasting other countries’ models for data governance without analyzing whether individual provisions, as well as the overall frameworks, are suitable for their specific country or their objectives.[64] The clearest reference models are the European Union, with its complex, onerous, and restrictive General Data Protection Regulation (GDPR), and China (with its restrictive “cyber sovereignty”). Countries often do this to save time, due to their attraction to certain parts of foreign models (such as government control of and access to data), and to pursue short-term goals (such as an EU “adequacy” determination to allow flows of EU personal data).
There is no “one-size-fits-all” approach to data privacy and protection, but there are common principles and processes, such as the OECD privacy principles.[65] This is where the focus should be. Each country’s data governance framework should be based on these shared international principles, but also reflect its own specific context, goals, and level of development. It would be costly (both economically and socially) for LMICs to think they have to replicate the EU’s approach before pursuing digital health and other objectives. LMICs should not have to wait to achieve a certain harmonized approach to data privacy before seeking to use and transfer health data. LMICs’ data protection frameworks should evolve alongside their efforts to pursue digital development, including for health outcomes. International health and development agencies should provide the resources and expert advice to help policymakers in LMICs find and enact the models that best fit their situations and objectives.
Facilitating Health Data Sharing and Access
To get the most out of health data, policymakers need to pay more attention to rules that facilitate the sharing of data. At the moment, most health data laws and regulations focus on individuals’ ability to restrict the use of their medical data, with scant attention paid to supporting their ability to share personal data for the common good.
Few countries have established norms and best practices for sharing health data. WHO’s 2015 Atlas of eHealth Country Profiles shows only 34 percent of surveyed countries have a legal or policy framework to manage the sharing of data through electronic health records (EHRs) between health professionals in the same country, and only 22 percent with regard to EHRs sharing between countries.[66] Furthermore, only 54 percent of countries have EHRs, which are a critical format for potential sharing.[67] Policies to support the sharing of data for research purposes are even rarer, with only 39 percent of countries having a framework to govern the sharing of personal and health data between research entities.[68] Only 17 percent of survey respondents had a strategy to govern the use of big data in the health sector.[69] This lack of governance only hinders the development and delivery of data-driven health solutions.
Figure 4: Countries allowing sharing of personal and health data between research entities (left) and between health professionals (right)[70]
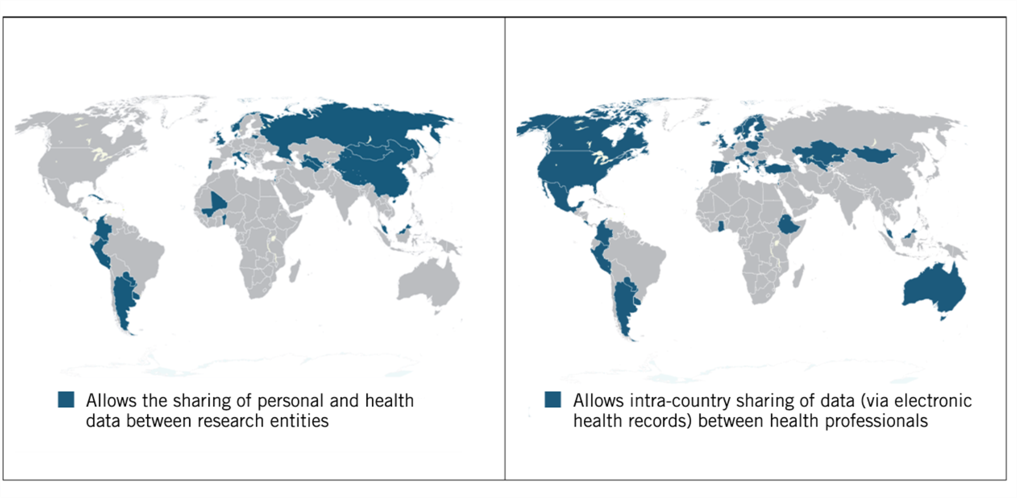
Indicative of this situation, the failure to share timely data was cited as one of the key impediments to mounting an effective response to the Ebola virus outbreak in Africa.[71] Governments and stakeholders had major issues trying to access and share call-data records (which include callers’ identities, the times of the calls, and the phone towers that handled them) during the outbreak.[72] Stakeholders ran into issues surrounding cooperation with phone companies, technical standards for requests, privacy protections, and contracts specifying who can access the data and for what use.[73] This is why countries and international organizations need to develop frameworks to facilitate the sharing of data at the regional and international levels before an international health crisis such as Ebola or COVID-19 emerges.[74]
Governments can also promote access and sharing of public data through “open-data” regimes.[75] A growing numbers of countries recognize the value in ensuring nonconfidential publishable data, including metadata, be made available free of charge online and in a format that is machine readable. By allowing open data, government agencies can foster data-driven innovation by government, private-sector organizations, civil society, academia, and individuals. Access to data has clear implications for health, particularly in the management of infectious disease outbreaks, and the allocation of resources according to factors such as disease prevalence, etc.
Open-data regimes can also maximize access to taxpayer-funded research data, ensuring it is available for reuse as quickly as possible. For example, in February 2013, the White House Office of Science and Technology Policy released a memorandum directing each federal agency with over $100 million in annual research and development (R&D) expenditures to develop a plan to increase public access to the results and data produced as a result of federally funded research.[76] Giving researchers access to study data as rapidly as possible helps maximize the benefits of data, allowing researchers to reuse the data for new research.[77]
Governments can promote access and sharing of public data through “open-data” regimes.
However, open data policies are still relatively new and underutilized in LMICs. For example, the progress of countries in sub-Saharan Africa toward enacting broad, consistent, and reliable open-data frameworks is slow overall and varied in practice (with cases of progression, but also regression, across the region).[78] Many countries lack the capacity, finances, or agreements to facilitate access to public and privately held data.[79] Open data in many LMICs is also hindered by state-centric cultures within which it is considered sufficient to have public institutions alone responsible for controlling and monitoring data collection.[80] Thankfully, LMIC policymakers have access to a growing range of supra-national institutions (such as United Nations agencies, the World Bank, and the African Development Bank) and NGOs that offer resources and advice specifically on open data and related issues.
Policymakers can also experiment with new institutional models, such as public-private partnerships, to improve data collection and access.[81] Governments can work cooperatively with private-sector firms on facilitating access to their specific country’s data so as to improve understanding of their nation’s residents, economy, and society—and their ability to address public policy issues, such as in health. However, absent some market failure, this needs to be done on a voluntary basis, given forced access to data would otherwise undermine the commercial incentive for firms to generate and use data in the first place. Policymakers need to partner with private-sector firms to ensure their proprietary, legal, and competition concerns are addressed.[82] Thus far, the structures for sharing such proprietary data are not standardized, so private data in most existing public-private partnerships is only made available on an ad hoc basis.[83]
Governments, especially public research agencies, can also encourage voluntary and mutually beneficial data sharing among private firms, researchers, and medical organizations—which may involve creating the technical architecture. For example, the U.S. Department of Health and Human Services (HHS) recently announced proposed new rules that would facilitate access to patient data by both patients and the health-care industry, in part by mandating the use of open application programming interface (APIs), which allow different software and databases to exchange data.[84]
Governments may need to step in to encourage firms in particular areas to voluntarily share data. Although there is a net benefit from data sharing to patients and researchers, there is not always a short-term benefit to companies for making their data available to their competitors. A model effort is the Accelerating Medicines Partnership, a U.S. National Institute of Health-led drug discovery collaboration among 10 drug makers, wherein participating companies have created a shared database that exceeds the capabilities of any individual company’s data holdings.[85] Similarly, some pharmaceutical firms have recognized that sharing is in their collective interest and have participated in data-sharing programs, including the Accelerating Medicines Partnership and a GlaxoSmithKline-led initiative to share patient-level clinical trial data with other participating pharmaceutical companies.[86] In other areas, such as medical device manufacturing, wherein data sharing has been a more difficult prospect, policymakers should conduct a review to identify factors preventing companies from sharing data with one another.[87] And HHS recently announced proposed new rules that would facilitate access to patient data by both patients and the health-care industry, by mandating the use of open APIs.[88]
Unfortunately, private-sector engagement in developing and creating these types of data-sharing frameworks and partnerships is very low in many LMICs.[89] There are examples wherein private-sector firms help provide data-driven insights that support health outcomes, such as MedAfrica using open data to improve access to health information. Similarly, the cell phone company Orange has an open-data challenge “Data for Development.”[90] Similarly, GovLab (based at New York University) helps different stakeholders—firms, research organizations, governments, and others—increase the availability and use of data by facilitating the exchange of data between different stakeholders.[91] It has facilitated dozens of projects that involve health-related data.[92]
Finally, policymakers should ensure patients themselves have access to the data they generate, and allow them to share it. At present, in most countries, there is no simple way for patients to contribute their personal data for use in medical research.[93] This type of policy tool, similar to the Blue Button initiative for general health data in the United States, would give individuals insights into their own health and allow them to authorize third parties to create applications using that data, which holds the promise of helping their health in the future through better treatments.[94]
These data-sharing efforts will help advance patient care in LMICs. Policymakers need to include these types of public and private data-sharing initiatives in their digital health strategies, as they will be crucial to achieving the end goal whereby respective parties can reasonably and responsibility access, share, and coordinate the full range of medical information—including medical histories, genomic data, behavioral data, and other sources—in order to provide better care to individual patients.
International Governance to Support the Protection, Flow, and Use of Health Data
International data governance that allows the movement of health data and services across borders will be crucial to building an integrated and effective global digital health framework. Just as diseases such as Ebola, malaria, and COVID-19 don’t stop at nations’ borders, health-care researchers and providers need to be able to effectively move data about these and other health challenges across borders in order to prevent and treat them.[95] The benefit of health data flows returns to the host country in the form of better, quicker, and cheaper health services and outcomes. Some examples of digital health programs that take advantage of the international flow of data are detailed in the appendix, for example Portal Telemedecina in Brazil, which uses cloud computing and AI to speed up diagnoses for patients living in remote areas; and U.S.-Chinese collaborations in using AI and machine learning to accelerate the process of drug discovery.
The following sections analyze the building blocks for an effective international health data governance framework: barriers to transfers of health data and the need to build interoperability between data protection frameworks.
Forced Health Data Localization Undermines Global Digital Health
Despite the significant benefits for companies, consumers, and national economies that arise from the ability of organizations to easily share data across borders, dozens of countries—across every stage of development—have erected barriers to cross-border data flows, such as data-residency requirements that strictly confine data within a country’s borders (a concept known as “data localization”).[96] Unfortunately, several countries have enacted barriers to the transfer of health data. This prevents firms from transferring data overseas for analysis or service delivery—as firms typically rely on cloud-based IT systems to provide services for operations around the world. Aside from explicit rules for local data storage, countries have also enacted de facto data localization requirements by mandating individual consent for cross-border transfers of data, thereby making them harder and more expensive, if not impractical and impossible.
Some examples of enacted and proposed data localization requirements that affect health data and related services include:
- In 2012, Australia enacted the Personally Controlled Electronic Health Records Act, which requires personal health records be stored only in Australia.[97]
- Two Canadian provinces, British Columbia and Nova Scotia, have implemented laws mandating personal data held by public bodies such as schools, hospitals, and public agencies must be stored and accessed only in Canada, unless certain conditions are fulfilled.[98]
- China has one of the widest sets of data localization policies in the world, including for personal, financial, mapping, and health data.[99] Most recently, in May 2019, China enacted rules that not only force firms to store genomic data locally, but also mandate all processing has to take place locally and by local firms—as foreign organizations are explicitly prohibited from managing Chinese genomic data.[100]
- India’s draft data protection bill permits the government to classify any sensitive personal data as critical personal data and mandate its storage and processing exclusively within India.This highlights the potential for localization, which would be consistent with both India’s recent decision to require localization for payments data and its potential application for other types of data.[101] Furthermore, for other types of personal data, firms must store a copy in India (known as data mirroring) before transferring data overseas (but only under certain conditions).
- In 2015, Russia enacted a Personal Data Law that mandates data operators that collect personal data about Russian residents must “record, systematize, accumulate, store, amend, update and retrieve” data using databases physically located in Russia.[102]
- Countries also enact de facto barriers to transfers of health and genomic data that make it harder and more expensive, if not impractical, for firms to transfer it overseas. For example, South Korea and Turkey require firms to get explicit consent from residents in order to transfer sensitive data such as genomic data overseas.[103]
Some policymakers use forced data localization policies in a misguided attempt to achieve enhanced privacy or security. The location of data can affect how organizations respond to lawful government requests for data. But controlling where organizations store data does not impact how organizations collect and use data (privacy), or how they store and transmit the data (security). The notion data must be stored domestically to ensure it remains secure and private is false.[104] With regard to security, while certain laws may impose minimum security standards, the security of data does not depend on the country in which data is stored, but rather only on the measures used to store it securely. With regard to privacy, data owners—whether they are individuals or businesses—rely on contracts and laws to limit voluntary data disclosures so data stored abroad receives the same level of protection as data stored domestically.
Beyond misunderstandings about data privacy and protection, some policymakers see data localization as a tool for “digital protectionism” that offers a quick way to force high-tech economic activity to take place within their borders—similar to how countries use local content requirements and tariffs to protect local manufacturing operations.[105] Given traditional trade-protection tools—such as tariffs—do not work as readily on digital economic activity, countries pursuing digital protectionism are reverting to “behind-the-border” regulations and technical requirements, such as data localization. One expected benefit is forcing companies to store data inside a country’s borders will produce a boom in domestic data-center jobs. In fact, while data centers contain expensive hardware (which is usually imported) and create some temporary construction jobs, they employ relatively few staff.[106] Data centers are typically highly automated, which allows a small number of workers to operate a large facility.[107]
The use of data localization is not only misguided, it’s actively harmful to a country’s economy and ability to facilitate innovation, as it’s likely to affect the price, availability, and range of all ICT services.[108] Localization of health and related data affects the cost and availability of countries’ health services and products—especially in LMICs, where the additional IT and operational costs of complying with localization more than likely outweighs the potential market opportunities, leading firms to avoid or leave those countries altogether. Small and medium-sized firms are the most affected, as they are the least able to deal with the cost and complexity of employing duplicative IT services in multiple markets. The impact goes beyond setting up or using a single data center, and whether firms want to deal with the complexity of setting up multiple centers for redundancy purposes and figuring out how (or if) they can adapt global data analytics platforms for local IT facilities (and how the two connect, or not). For example, IBM Watson—which combines a supercomputer, AI, and sophisticated analytical software—requires customized hardware for each application (such as health), so it is unrealistic to assume IBM would deploy an independent Watson application in each and every country that enacts barriers to transfers of health data.[109] As firms weigh the cost-benefit of entering a particular market, data localization will increasingly be a factor.
Diseases and viruses (such as COVID-19) do not stop at national borders, meaning data needed to find cures needs to cross them.[110] The presence of localization influences if and where firms conduct clinical trials and data-driven health research. Powerful data analytics applied to bigger global datasets helps speed the development of cures.[111] The rarer the diseases, the more important it is to build bigger datasets. By erecting barriers to the exchange of medical information—even anonymous data—countries’ protectionist policies harm not only their own residents, but also people around the world, all of whom benefit from advances in medical research that may be possible from the aggregation and analysis of health and genomic data.
Interoperability Is the Key to Functionality, Cooperation, and Scale
International interoperability between different countries’ data governance frameworks—thus allowing information, and the digital products it represents, to move between jurisdictions—is important in maximizing the benefits of health data. These data flows allow organizations to aggregate larger, more valuable datasets for research, and leverage cloud storage services to deliver health services across borders. For firms involved in developing and delivering digital health products, international interoperability is critical to their competitiveness, as it builds economies of scale. For policymakers and individuals, this means greater health-sector competition, and access to a larger range of health services. This is why policymakers need to think regionally and globally when looking at domestic digital health and data governance policies.
Within digital health, interoperability at the domestic level refers to technical and legal issues that make it difficult for different organizations to collect, share, and analyze data because they often exist in non-standardized formats and reside across isolated databases and incompatible software systems. This is a related, but separate, issue to international interoperability within digital health. The objective of improved domestic interoperability is to ensure seamless communication across different IT systems through common data standards, which is similar to international interoperability, except it is to ensure data transfers between different countries.
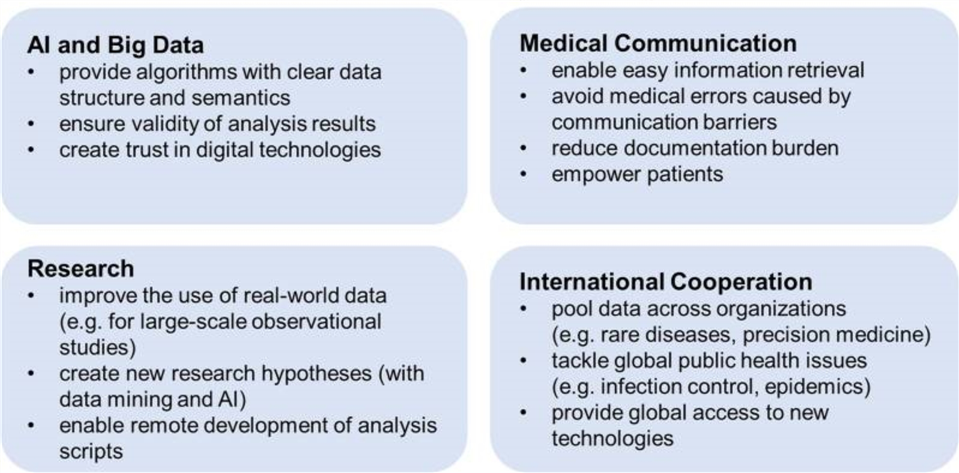
Data localization needs to be avoided as businesses use data to create value—and many can only maximize that value when data can flow freely across borders. The movement of data is crucial to the application of AI and big data for innovative health and drug research, the generation and use of real-world data from personal devices such as smart watches, international virus and disease surveillance, the remote delivery of health services to smart phones via apps, and doctor-patient communications (see figure 5). In the case studies, the many firms and organizations that operate across multiple countries show how cross-border data flows are essential to their operations.
Figure 5: How interoperability improves digital medicine[112]
Policymakers need to ensure domestic data governance rules not only allow, but facilitate the cross-border transfer and sharing of health data. As noted previously, only 22 percent of countries allow the sharing of EHR data between countries, and only 39 percent of countries allow the sharing of personal and health data between research entities.[113] Given EHRs are one of the core and most-common types of health data, this shows more countries need to ensure they allow sharing of critical health data.
Policymakers need to ensure domestic data governance rules not only allow, but facilitate the cross-border transfer and sharing of health data.
A major barrier to greater sharing of health data in LMICs is their lacking in technical expertise and understanding about the tools, standards, and regulations required to facilitate interoperability, as the Pathways for Prosperity Commission’s report on digital development shows. In interviews, senior developing-country officials stated that technical assistance is one of the best ways the international community can help developing nations get the most from digital technologies.[114] Just as governments and stakeholders need to invest in physical ICT infrastructure, training programs, and other foundational areas to support the digital economy, so too do they need to invest in governance and ecosystem design.
The European Union: Pursuing Domestic, But Not International, Interoperability
The European Union pursues a differential and conflicting approach—interoperability within and between member countries—while making it much harder to transfer data between the region and the rest of the world.
The European Commission enacted several other policies to improve EU interoperability and standardization in health care. For example, the European Commission’s eHealth Action Plan 2012–2020 aims to facilitate the use of ICT to improve health care in Europe, including by focusing on developing common standards to enhance interoperable health-care systems among member states. Also, during the period 2013–2020, the commission is using funding from the Connecting Europe Facility and the European Regional Development Fund programs to push for a large-scale diffusion of innovative tools, the replicability of good practices, and services for health, aging, and well-being—with a particular attention on improving equal access to services.
The problem is the EU’s approach to global data governance is based on harmonization (and not interoperability), as it only wants EU personal data to be able to move to a small group of other countries that essentially have the same onerous and highly restrictive data protection regulation (i.e., the GDPR).[115] The EU has thus far deemed a disparate group of 12 countries (mainly former colonies) as providing an “adequate” level of protection as compared with the GDPR. Firms wanting to transfer data to other countries have to use legal tools that are costly and complicated, especially for small and medium-sized firms.
Interoperability should be a core feature in each country’s domestic data governance framework, as the globally distributed nature of the Internet means a country’s laws need to be global in scope and interoperable in practice. Interoperable data governance frameworks are the international extension of the accountability-based approach this report recommends, as the data is still able to flow between different privacy regimes, while countries’ data protection rules flow with it. However, while each country adopts its own data governance framework, there can be shared and mutually recognized principles, norms, and processes. For example, OECD privacy principles identify global interoperability as an explicit goal, which has been embedded in many countries’ privacy laws.[116] As LMICs develop their national digital health strategies, there is an opportunity to adopt this interoperable principle into their framework from the beginning. This is the approach adopted by Vietnam (as detailed in the appendix), which is using its transition from paper to EHRs to adopt a modern standard that will make its system more reliable, safe, quick, and future proof.
Interoperability can feature in accountability-based data governance frameworks in several ways. It can come in the form of legal requirements that ensure firms and their subcontractors adhere to domestic data-handling requirements even when processing data outside the country. Firms can mitigate these risks by stipulating requirements in relevant data-handling and processing contracts they implement with other companies, and implement (and demonstrate) accountability through various internal privacy and information management programs, regulated frameworks (such as the EU’s Binding Corporate Rules), industry codes of conduct, third-party certifications and seals, and international standards.[117] For example, foreign companies operating in the United States must comply with the privacy provisions of HIPAA—which regulates U.S. residents’ privacy rights with regard to health data—even if they move data outside the United States. And, if a foreign company’s affiliates overseas violate HIPAA, then U.S. regulators can bring legal action against the foreign company’s operations in the United States.
Countries and regions can also enact data-transfer agreements to facilitate international interoperability, as in the EU-U.S. Privacy Shield and the Asia Pacific Economic Cooperation’s Cross-Border Privacy Rules (CBPR). However, while useful, the Privacy Shield is needed as the EU’s general approach to data governance does not promote interoperability, but harmonization, as it wants all other countries to adopt its onerous and restrictive approach to privacy. The European Union also tries to make foreign countries responsible for enforcing European data privacy standards instead of relying on their own legal systems to uphold those standards if that is what they are contractually obliged to do.
The CBPR is a good example of an interoperable framework for the cross-border transfer of personal data.[118] CBPR was established in 2011 and is based on the APEC Privacy Framework launched in 2005 (updated in 2015), which provides a principles-based system for national privacy laws that recognizes the importance of “effective privacy protections that avoid barriers to information flows.”[119] Australia, Canada, Chinese Taipei, Japan, Mexico, Singapore, South Korea, and the United States have all signed on to the CBPR. The CBPR is a voluntary, accountability-based system that facilitates “privacy-respecting” data flows across borders. CBPR-compliant firms are able to transfer (both inter- and intra-company) personal data across borders. The CBPR system requires participating businesses to implement data privacy policies consistent with the APEC Privacy Framework, such as those regarding accountability, notice, choice, collection limitation, integrity of personal information, uses of personal information, and harm prevention. The participating economy appoints an APEC-approved third-party agent to audit and certify that companies have compliant data-privacy policies. Countries are drawn to it partly because it is not prescriptive or specific to any particular policy framework or political system, and is focused on addressing core issues and processes around providing a clear and consistent regulatory framework for firms managing personal data across the region. What CBPR helps ensure is a country’s privacy rules travel with the data, and a company can commit to abide by these rules, wherever it stores the data. CBPR also helps ensure a country’s privacy rules are enforced.[120]
Looking ahead, LMIC policymakers and their partners need to recognize that the cross-border governance of technology is unlikely to be governed by one all-encompassing digital economy framework. For example, there will not be a single, harmonized approach to data governance. However, there are clearly common principles and shared interests and benefits from greater cooperation. As the Pathways for Prosperity Commission’s report The Digital Roadmap: How Developing Countries Can Get Ahead advises, it’s better for motivated countries to push ahead with like-minded neighbors and other stakeholders in coordinating digital policy wherever cross-border spillovers are more immediate, or the efficiency gains from acting together are greater.[121] LMIC policymakers and their partners, such as regional development banks, should identify opportunities for like-minded neighbors to work together on these policies to build both domestic and regional interoperability and improve digital health outcomes for patients in all participating countries.
Multilateral Governance and Support of Digital Health
In recent years, digital health has emerged as a key agenda item for international health and development agencies as they recognize the important role digital technologies can play in supporting better health outcomes, especially in LMICs. E-commerce negotiations at the World Trade Organization (WTO) by 70-plus countries also have the potential to achieve new rules that would support the flow of health data and the cross-border provision of health services.[122] This section summarizes leading multilateral efforts to improve digital health outcomes around the world.
The Emerging Global Framework for Action: WHO and Others Ramp Up Work on Digital Health
2018 signaled digital health’s emergence as a major issue on the international stage, as WHO and several other agencies and stakeholders increased their work on the issue. COVID-19’s emergence in 2020 is no doubt accelerating efforts to embrace digital technologies for health given the role smartphone apps and other digital tools have played in helping to control the spread of the virus.[123] Consider also the broader role emerging digital technologies such as 3D printing have played in producing personal protective equipment.
In the last few years, WHO has laid a foundation of work to build on in developing a more coordinated, comprehensive, and effective global approach to digital health. But as this report and the reaction to the COVID-19 pandemic show, considerable work remains. In 2018, member countries ratified WHO Resolution WHA71 A71, which aligns the use of technology with the achievement of the United Nation’s Sustainable Development Goals (SDG), including SDG 3: Good Health and Wellbeing. The resolution calls for advancements across a range of digital health themes, including support for national and global health priorities, promotion of interoperability, sharing of best practices, and digital health workforce development. This resolution also calls on WHO to develop a global digital health strategy to, inter alia, provide technical assistance and normative guidance to member states and develop a repository of regulations, evidence, and best practices. A draft was published in March 2019 entitled WHO’s “Global Strategy on Digital Health 2020–2024.”[124] Its vision is to, “improve health for everyone, everywhere by accelerating the adoption of appropriate digital health.”
Its four strategic objectives are:
- Committing to a shared global agenda: The UN organization will work to engage stakeholders, including government officials, health-care organizations, ICT providers, researchers, and patients.
- Building a global digital health capacity specific to individual nations’ needs.
- Advancing digital health in every country.
- Improving digital health measurement, monitoring, research, and practice.
In October 2019, WHO’s “Digital Health Technical Advisory Group” met for the first time to help build a roadmap to advance the digital health ecosystem.[125] Most recently, this group convened a virtual roundtable with technology experts to help advance WHO’s collaborative response to COVID-19.[126] It will reportedly try to address many issues, some of which are identified in this report. However, its membership is unclear, so it’s unknown whether it will include a cross-section of representatives, including the private sector and non-health experts in data governance, innovation, and trade. The remit of the advisory group includes:
- developing a global framework for WHO to validate, implement, and scale up digital health technology and solutions;
- recommendations for the safe and ethical use of digital technologies to strengthen national health systems by improving quality and coverage of care and increasing access to health information;
- advice on advocacy and partnership models to accelerate use of digital health capabilities in countries to achieve better health outcomes; and
- advice on emerging digital health technologies with global reach and impact, so no one is left behind.
WHO efforts are supported by a range of other emerging initiatives that aim to help LMICs get the most from digital health. For example, in February 2018, a group of 13 national governments, digital health agencies, and WHO established the Global Digital Health Partnership.[127] The 13 countries in the partnership are Austria, Australia, Canada, India, Indonesia, Italy, New Zealand, Saudi Arabia, Singapore, South Korea, Sweden, the United States, and the United Kingdom. The aim is to share policy and evidence that supports members to deliver better digital health services. Later in October 2018, the Donor Alignment Principles for digital health were launched at the World Health Summit in Berlin to promote country ownership and leadership, and pool funding across donors to support national-led efforts.[128] In the same month, the United Nations Children's Fund (UNICEF) Office of Innovation published its “Approach to Digital Health,” which provides guidance on how digital technologies can be used to further the goals of UNICEF’s Strategy for Health 2016–2030.[129]
These initiatives follow the comprehensive and useful report “Digital Health: A Call for Government Leadership and Cooperation Between ICT and Health” published by the Broadband Commission for Sustainable Development (a joint initiative by ITU and UNESCO).[130] One of its working groups on digital health also published a report examining the role of digital health in relationship to non-communicable diseases, including diabetes.[131] Finally, and more recently (2019), the Pathways for Prosperity Commission published a well-researched and constructive report entitled The Digital Roadmap: How Developing Countries Can Get Ahead.[132]
It is certainly a huge challenge to improve LMIC’s use of digital technologies for better health outcomes, especially given the economic and financial impact of COVID-19 on what are often already under-resourced and struggling health systems. However, this underlines the imperative for LMIC policymakers and their international partners to pool their limited resources and expertise in an effective, coordinated, and targeted manner in the years ahead.
Recommendations
Digital health technologies hold great potential to improve health outcomes around the world—especially in LMICs. To maximize the benefits of digital health technologies, policymakers and stakeholders will need to take a holistic approach that addresses key enablers at the national, regional, and international levels.
The following are this report’s main, general findings and recommendations:
- Countries should develop holistic national digital health strategies. To be effective, such plans require political leadership, whole-of-government participation, and multi-stakeholder engagement. There is wide disparity in progress in this area among LMICs, with several important countries having no formal national plan. International organizations should continue to develop shared templates and strategies that can be adopted by LMICs.[133]
- Training and education in digital technologies are critical, but few developing countries have integrated digital skills into their health-workforce training. Regional and multilateral health organizations, donors, and other stakeholders should prioritize efforts to develop a more coordinated strategy and set of pragmatic best practices to help LMICs quickly address the most pressing skills gaps that prevent them from benefiting from digital technologies.
- There are particularly acute gaps in ICT infrastructure in LMICs, which are home to most of the people that remain disconnected from the Internet. This means the benefits of digital technologies—including for health—remain out of reach. Regional and multilateral development agencies, and other donors, need to devote greater attention and resources to closing these gaps—such as wireless mobile coverage in rural and other hard-to-reach places—in ICT infrastructure.
- Too many developed countries have data governance frameworks that are overly restrictive or do not facilitate data sharing, both of which limit the potential benefits of digital health technologies. The risk is that LMIC’s emulate this approach. Instead, LMICs should enact data governance frameworks that balance data privacy, protection, and innovation. The generation, protection, use, sharing, and international transfer of health data is critical to building an effective digital health program.
- LMICs and their international partners need to build interoperability within their digital health systems from the start. Many benefits of digital health technologies require cross-border flows of data. There is a real risk policymakers in LMICs will misguidedly force firms to store health data locally on the mistaken basis it makes data more secure and private or because they think only local firms should have access to it (which limits health services and outcomes). Instead, policymakers should embrace an accountability-based approach to ensure a country’s data protection rules travel with the data, wherever it is stored, so residents can benefit from new digital services, whether they are provided from home or abroad.
Conclusion
Domestic and international policymakers are only in the early stages of putting in place the principles, policies, and frameworks that would provide the supporting structure for broad and consistent cross-border engagement. COVID-19 shows the necessity for greater collaboration on health issues, the power of data and digital tools, and the need for targeted digital health strategies to help countries, regions, and the world get the most out of digital technology tools. Without the right strategies and technical and resource support, the gap in the digital divide will become increasingly evident in terms of developing country health outcomes.
Appendix: Case Studies Showing How Digital Health Can Help LMICs
The appendix features 13 case studies of digital health applications improving health outcomes in several developing countries, including Brazil, China, India, Indonesia, Rwanda, Saudi Arabia, South Africa, Vietnam, and Zambia.
Brazil: Remote, Rapid Diagnosis Using the Cloud and Machine Learning
Like many large, middle-income countries, Brazil has a large rural population that is poorly served by existing health-care infrastructure. Clinics are few and far between, and in particular there are shortages of specialist physicians serving populations outside of cities.
Portal Telemedicina is a Brazilian company that has pioneered the use of telemedicine to allow doctors from underserved communities to work more closely with medical specialists based in other parts of the country. An added innovation from the company is the use of AI and machine learning to speed up diagnoses, allowing doctors to send virtual reports to hospitals in any Brazilian location in real time. The website is live 24/7, and gives patients access to a range of medical specialists.
In sum, Portal Telemedicina brings medical specialists from the cities to the countryside, without anyone having to get on a plane, bus, or train.
For such a platform, data and patient confidentiality is key. The company has partnered with Google to encrypt patient information and store it in the cloud. Portal Telemedicine also uses Google tools to train its algorithms to detect certain diseases based on test results. This allows for automatic triaging and the allocation of cases based on clinical need and priority. Specialists can thereby ensure the most pressing cases are seen first.
This automated process massively reduces the time it takes to receive a diagnosis. Under a traditional system, it can take days for a test to be administered, analyzed, and the results delivered back to the physician. Portal Telemedicina can deliver test results to some of the best specialists in Brazil in just a few minutes. Using the cloud to deliver services has also slashed hospital operating costs.
The application has potential beyond Brazil. According to Rafael Figueroa, cofounder and CEO of Portal Telemedicina, "We are growing and operating at large scale thanks to Google Cloud. Today, we generate around 3,000 reports daily, with a team of 30 doctors…. Apart from Brazil we also provide services to Angola, in Africa, and we are planning to expand our reach to the US and Europe."[134]
China: An Emerging Global Center for the Use of AI in Drug Discovery
“Right now, China is experiencing a ‘Cambrian explosion’ in biotechnology. Many top scientists from pharma and academia moved back to China and started working on known targets,” according to Alex Zhavoronkov, founder of Insilico Medicine, a U.S. biotech company that combines genomics, big data analysis, and deep learning for drug discovery.[135] As ITIF has written, China seeks to displace the United States as the world’s life-sciences innovation leader.[136]
China has identified AI as a strategic national industry, and the government is keen to leverage its potential to help improve capacity and productivity within the country’s health-care system, which faces a looming crisis both from the country’s rapidly aging population and an acute shortage of qualified doctors. In 2017, China released its “AI Strategic Plan” that outlines the ambitious goal of making the country the undisputed world leader in AI by 2030.[137] The government has also recently issued a strategic plan Made in China 2025, under which the country looks to heavily invest in R&D to boost innovation.
Chinese companies from start-ups to tech giants are seizing the opportunity to apply AI solutions to everything from machine reading of CAT scans to processing and analyzing medical queries. The Chinese health-care big data industry is worth over $11 billion as of 2020, with hundreds of Chinese-based AI ventures emerging every year, according to the South China Morning Post.[138]
According to GlobalData, a key area of China’s current focus is machine learning algorithms, which help reduce R&D cycle times and costs.[139] This ultimately allows companies to have a strong and sustainable drug pipeline while also increasing their trial completion rates.
On the deal front, San Francisco’s Atomwise and China’s Hansoh Pharma announced in September 2019 an AI drug discovery deal that could be worth $1.5 billion (the largest U.S.-China collaboration in the field). The deal is to design and discover potential drug candidates for up to 11 disclosed target proteins in several therapeutic areas.
In October 2019, Insilico Medicine signed a dual-program discovery collaboration with Jiangsu Chia Tai Fenghai Pharmaceutical worth up to $200 million, focused on previously undruggable targets in triple-negative breast cancer.[140]
In November 2019, AstraZeneca announced the establishment of a new AI Innovation Centre in Shanghai to capitalize on the latest digital technology in R&D, manufacturing, operations, and commercialization in order to accelerate the delivery of medicines to patients both in China and globally. A dedicated group within the institute will focus on collaboration with technology companies and local start-ups to develop innovative solutions for patients.[141]
India: Helping Tuberculosis Patients While Providing Essential Data to Public Health Officials
Source: Adapted from health is the NGO PATH’s case study “Finding the Missing Millions: The Importance of Private Sector Engagement for Eliminating Tuberculosis.”[142]
Tuberculosis (TB) is highly infectious, which is especially problematic in crowded cities within developing countries, such as in Mumbai, India, where many people have no access to government health-care facilities and instead rely on private-sector providers (as 70 percent of TB patients in India do). TB is curable when a patient takes drugs as per schedule. However, many people do not follow the prescribed treatment regimen or drop out entirely and end up being infected by TB multiple times. This leads to the building up of drug resistance. Also, TB patients being treated at private providers often goes unreported to the government, which thus has a limited view of the issue.
The Indian government, WHO, and PATH set up a high-tech TB treatment program—the private provider interface agency (PPIA)—to reduce the burden of TB in urban centers. The program gives TB patients in the private sector access to free public-sector medicines and state-of-the-art diagnostic services. PPIA uses the power of data and ICTs to connect public and private health-care providers. It deploys digital technologies such as text message reminders, connected patient databases, and custom apps to deliver better health care for urban populations.
PATH’s program is based around a central database and e-voucher system that offers three advantages: easy referrals, more robust patient tracking, and seamless payment and reimbursement.[143] It works in the following way: Patient referrals and subsidies are managed through e-vouchers that guarantee payment to private providers and pharmacies. A call center connected to the database runs the voucher program and supports patients to complete the full course of treatment. The database also makes it easier for PPIA staff to contact patients (via text and phone calls) in order to ensure they’re adhering to their treatment plans. Because pharmacists—in addition to doctors— are trained to use the voucher system, drug refills are also tracked to ensure compliance. Field workers provide additional personalized outreach, motivating patients to finish the long and difficult treatment regimen. Behind it all, decisions based on real-time data promote seamless program operation and improved patient outcomes.
PPIA’s unique ICT tools have been very effective. PPIA reduced diagnosis time by 43 percent for less-than-fully qualified practitioners, and 30 percent for fully qualified practitioners.[144] PPIA was able to increase private-sector case notifications in Mumbai from 2 percent (3,000) of total notifications in 2013 to 47 percent (22,260) in 2017.[145] This patient-centered, technology-intensive model has resulted in a treatment success rate above 80 percent. Based on this success, a version of the program called JEET (Joint Effort to Eliminate Tuberculosis) is currently being rolled out broadly across India, and is projected to impact 3.5 million people across 22 states and 400 cities in the next 2 years.
The tools have also enabled quicker entry of case notifications from the private sector into public-sector health systems, and made it possible to capture events in patients’ individual pathways through the end of treatment, which when aggregated, provides population-level insights into treatment adherence. Given this, the government decided to include these ICT tools as part of a country-wide notification system. India now has a clear path forward to find and treat the estimated 1 million undiagnosed cases of TB in the country using technology to link health sectors.
India: Using Artificial Intelligence to Prevent Blindness in Diabetics
Diabetic retinopathy is a kind of nerve damage in eyes that, if not detected early, can lead to blindness. As lifestyles and diets continue to change in India, it is becoming an increasingly serious threat to eye health. It’s estimated there will be 11 million to 20 million people with diabetic retinopathy by 2025, including 5.7 million people with severe retinopathy, in India.[146]
In India, where there are insufficient numbers of clinics and specialists, many patients—up to 45 percent according to some estimates—suffer vision loss before they can be diagnosed.[147]
AI offers the potential to reverse this situation by providing faster diagnoses using fewer resources. Google and several Indian doctors are working together to use AI to speed up and lower the cost of diabetic retinopathy diagnosis, thereby making it accessible to far more people.
Google has developed an AI model that can detect diabetic retinopathy by analyzing the scans of retinas using special cameras. This image is then analyzed by Google’s machine learning algorithm, which then grades those scans on a five-point scale ranging between no diabetic retinopathy, which can be managed using a combination of diet and medication, to the most severe case, which may require surgery.
“In 2016, we published a paper in the Journal of American Medical Association showing that this AI system was performing the level of the Generalists. Since then we have made improvements to the algorithm, and now it is on par with the specialists,” Google product manager Lily Peng said at the company’s Solve with AI Conference in Tokyo in 2019.[148]
Google has piloted the program in Thailand and India, where it partnered with Aravind Eye Hospital in Madurai and Sankara Eye Hospital in Chennai. The latter runs around 70 satellite clinics that cater to patients who cannot travel into the nearest town. At these clinics, the images of the patients’ retinas are taken and then uploaded to Google Cloud. From there, Google’s ML algorithm works in combination with specialists to detect and diagnose the disease, which can then be treated based on its severity.
Google is not the only company in India to be working in this field. Forus and Remedio have also developed devices that can detect diabetic retinopathy at early stages. Zeiss’s Bangalore-based MedTech R&D center CARIn has also developed an AI-powered solution that uses a machine learning algorithm to detect diabetic retinopathy.[149]
Indonesia: A Web Platform for Clinician and Patient Interaction
Source: Adapted from Tech Collective’s case study, “Exploring Indonesia’s Healthcare Startup Scene”[150]
The Indonesian firm Atoma Medical operates one of the country’s health digital communication companies (based on its website “TanyaDok”), which is a question-and-answer platform run by doctors and medical professionals to provides health-care information. TanyaDok’s goal is to become the sole hub connecting all the dots in the Indonesian health-care sector. Since 2006, the site has been supported by a medical editorial team and hundreds of contributing doctors including general physicians, dentists, and an array of experts, such as specialist doctors and senior consultants. It also acts as a central hub for patients to arrange online consultations with a network of health-care providers. Its founder, Gregorius Bimantoro, identified three of the most crucial issues his company aims to solve: disparity between the number of doctors available to treat every citizen, lack of access to information, and availability of products and services.[151]
TanyaDok has managed to secure 700,000 monthly page views and 1 million total users and a network of over 200 doctors.[152] The portal estimates having given tens of thousands of consultations, either via email or social media, with doctors reporting around 20 to 50 consultations per day. A paid-premium membership enables doctors to have access to the users’ medical records for a more personalized and in-depth consultation. Each doctor’s consultation is restricted to giving medical advice on the patient’s complaints. TanyaDok is working on partnering with Network Health Services (ranging from hospitals and specialist clinics to clinical laboratories, etc.) to provide users with continued service, with the goal of offering home care services to paid-premium members.
Indonesia: Combining Mobile Technology and Physical Health Infrastructure to Improve Access to Health Care
Halodoc is an Indonesia-based health-tech mobile-application platform that combines two separate services: tele-consultation with health-care professionals, and the delivery of pharmaceuticals in 30 cities across Indonesia. It is currently used by about 40 million people to connect with more than 22,000 licensed doctors in the country. The firm hopes to expand its coverage to 100 million people, representing nearly 40 percent of the Indonesian population, in the next year.[153]
Halodoc shows how digital solutions can be used to make more-efficient use of existing physical health resources, particularly for areas where facilities are scarce. By making it more available and affordable, Halodoc is contributing to the goal of achieving universal health care.
Such mobile technologies offer a sustainable and cost-effective solution to some of the biggest barriers to health-care access in rapidly urbanising, large, developing countries such as Indonesia. On the one hand, in megacities such as Jakarta, levels of traffic are such that it can take many hours to simply make it to a medical appointment. For the many people who live in rural areas, health-care facilities and doctors are few and far between. It’s often impossible for people to get quick and affordable access to medical care. Indonesia’s population of 260 million is spread across 17,000 islands. It has only 2 physicians for every 10,000 people (fewer than the 8 in India and 26 in the United States) according to the World Bank.[154] Public health facilities and the road network both operate beyond capacity, resulting in queuing and shortages.
Halodoc represents a technological solution to the twin problems of shortages of health-care professionals and a congested network. Users of the app can log in for an online video consultation with a physician, who is able to issue prescriptions via the app to be fulfilled by 1 of the 1,000 or so pharmacies in the Halodoc network. Finally, Halodoc arranges for the prescriptions to be rapidly delivered by motorbike or scooter. The platform deploys AI and machine learning-based solutions to create efficiencies, cost savings, and a distinct competitive edge.
Physician consultations start at 25,000 rupiah (or $1.75) for a 10-to-15-minute consultation—which is lower than the average cost at a traditional primary clinic—and the company aims to deliver prescriptions within 40 minutes.[155]
Further enhancement of the Halodoc services comes through its partnership with 1,400 hospitals and health-care providers. Halodoc users benefit from avoiding queues at pharmacies post-appointment, and a reduction in costs via automatic linking with the their individual insurance company. This makes for a seamless, cashless transaction. In October 2019, Halodoc signed a memorandum of understanding with the national health insurance scheme BPJS Kesehatan to provide digital-based health services through the BPJS mobile app. This further expands the user base and brings a new suite of capabilities, including preventative health advice.
Indonesia: Mobile Obstetrics Monitoring Through an App and Software Project
Source: Adapted from Philips company blog post, “Monitoring Pregnancies Using Mobile Solutions”[156]
Indonesia has a significant problem with maternal mortality, standing at 126 per 100,000 live births in 2015, well above the United Nations Sustainable Development Goal target of less than 70 by 2030. Given most deaths occur in rural areas where there is a shortage of staff and facilities—but within cell phone coverage—mobile technology is turning out to be an effective tool to reduce maternal mortality. Indonesia has mobile penetration of 79 percent of the population and the fourth-largest smartphone user base in the world. Midwives and doctors also have personal technology skills that support the adoption of smartphone-based solutions.
In 2018, Philips partnered with Bunda Medical Center in Padang, West Sumatra, (one of the leading hospitals in Indonesia in the area of pregnancy) to address problems during antenatal care using the Philips Mobile Obstetrics Monitoring (MOM) solution. This partnership was a collaboration between Bundamedik, the city government of Padang, the Indonesian Ministry of Health, and Philips Healthcare. The app enables midwives to build a pregnant woman’s health profile by collecting data from physical examinations, tests, and local nursing clinics—or even from soon to-be mothers’ homes. Data is uploaded from the app to the central MOM server, allowing obstetricians and gynecologists to remotely monitor patients from hospitals or home. Doctors can review the data collected from the antenatal visits and determine whether individual pregnancies might be high risk, in which case immediate care can be provided.
Figure 6: Mobile obstetrics monitoring
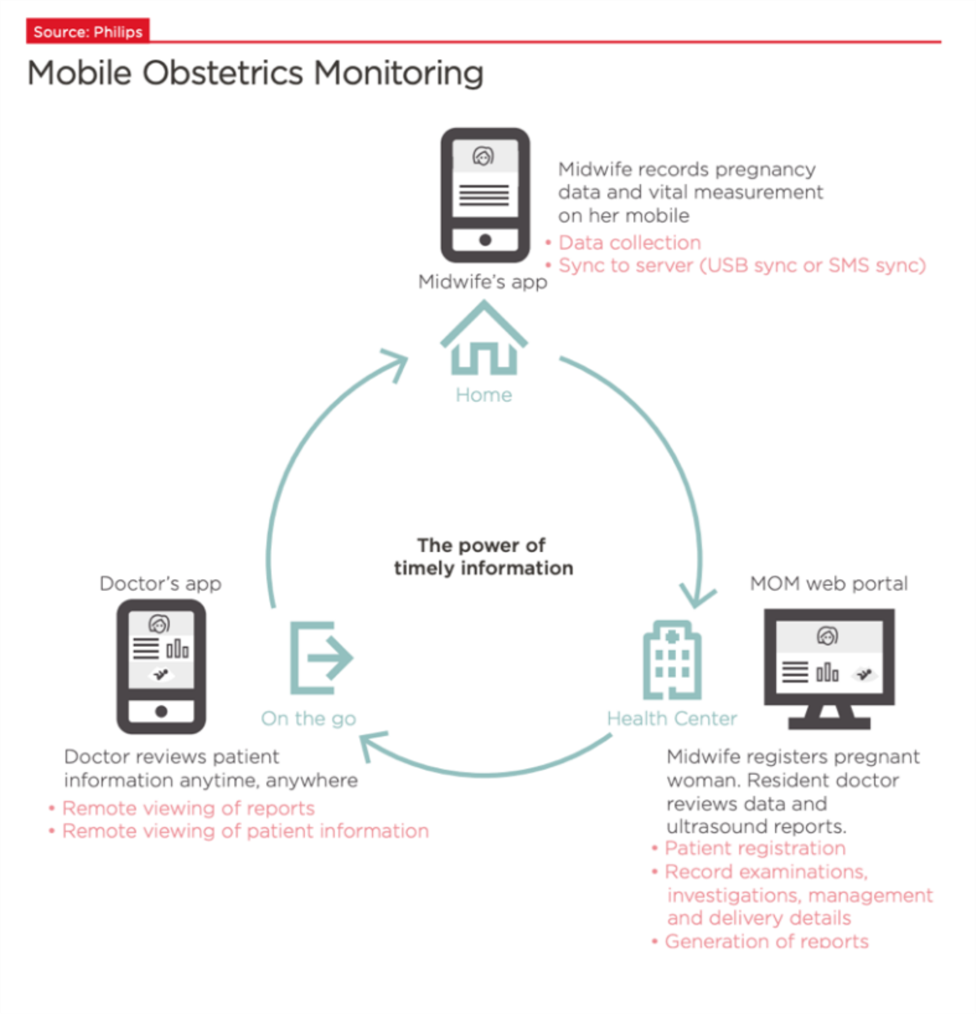
MOM also features training and education services for health-care workers, as well as a protocol of antenatal care to guide caregivers. The tool includes a clinical decision system to guide users in assessing the risks to the pregnancy. In the first year, the pilot project involved more than 650 pregnancies. MOM increased the early detection of high-risk pregnancies threefold. No women died from preventable causes related to pregnancy and childbirth. There was also a 99 percent reduction in anemia from the first to the third trimester through early identification and enhanced patient management.
Rwanda: App-based Patient Consultations That Use Artificial Intelligence and Machine Learning
Rwanda suffers from a very low number of health professionals, estimated at around 1 per 12,000 people in the country.[157] By contrast, Rwanda enjoys extremely high levels of mobile phone penetration at around 80 percent.[158] This provides an opportunity to use mobile technologies to improve access to health care.
In September 2016, the Rwandan Ministry of Health partnered with London-based start-up Babylon Health and the Bill & Melinda Gates Foundation to launch a mobile phone app that gives residents instant, free access to expert health advice.
The app allows users to connect to a chatbot that uses machine learning and AI to triage medical problems. It offers simple treatments for basic medical problems, and whenever it recognizes a condition is more serious, it sets up an appointment to chat with a real physician by phone or video. Consultations are extremely cheap for patients, costing only around $0.65, while patients without access to a mobile phone can visit babyl booths equipped with tablets and phones at various pharmacies.
Babyl is staffed by a team of 25 doctors—who speak English, French, and Kinyarwanda—employed at government hospitals. The doctors provide basic diagnoses and further treatment recommendations, and issue prescriptions direct to users’ mobile phones.
“It's about giving a patient quick access to a doctor,” explained Shivon Byamukama, M.D., deputy CEO of Babyl Rwanda. “In the end, what you need is a doctor’s brain, not the brick and mortar that comes with a hospital.”[159]
In 2 years, more than 2 million Rwandans, or 30 percent of the population, have registered to use the app. Five hundred residents of rural villages are employed as Babyl ambassadors to introduce their community to the service. In its first year, Babyl Rwanda has had 600,000 registrations and more than 100,000 consultations.
Babylon has confirmed it’s planning to launch its service in more countries, with Digital Health News reporting in April 2018 the company had partnered with the Chinese Internet company, Tencent, to help deliver personal health assessments and treatment advice across mainland China.[160]
Saudi Arabia: Digitization of the Pathology Workflow Improves Care and Lowers Costs
The Kingdom of Saudi Arabia is steadily moving to build a digital health ecosystem as a key pillar of its Vision 2030 program. The Ministry of Health aims to have digital records for nearly 70 percent of Saudi residents by 2020. In addition, there are plans for digital health-care tools to further enhance the performance and productivity of health-care providers, thereby facilitating the delivery of high-quality services.
“As data begins to be gathered robustly on the prevalence of diseases and segmentation of patients becomes possible, proactive targeting of patients can be realized. Using technology to drive these interventions, such as digital behavioral management programs supplemented with offline care management systems will achieve better outcomes and better patient satisfaction,” according to Emmeline Roodenburg, head of Healthcare, KPMG Saudi Arabia.[161]
As one example of the potential of digital services to transform patient care in the kingdom, global health technology firm Royal Philips and Al Borg Medical Laboratories, the largest chain of private laboratories in Saudi Arabia, have partnered to fully digitize the diagnostic process for patient tissue examination.
In Saudi Arabia, 85 percent of cancer malignancy confirmations are based on manual histopathology reports.[162] Each tissue slide needs to be prepared, analyzed through a microscope, diagnosed, reported, and archived. If a patient wants to seek a second opinion, they must ship or hand-deliver the slides to a second pathologist, which carries the risk of slides being lost or damaged in transport.
The digitization of the pathology workflow provides specialist pathologists with remote access in order to review tissue samples with the goal of offering patients a precise and faster diagnosis. Pathologists can then review, interpret, analyze, and easily share these digital images from any location and by more than one person at a time through the Image Management System, allowing pathologists to quickly consult a specialist, or conveniently share images during multidisciplinary team meetings without physically transporting tissue samples.
“The digitization of pathological diagnostics provides an opportunity to radically change the way that complex diseases like cancer are diagnosed by improving collaboration among pathologists and enhancing their daily workflows,” said Marlon Thompson, general manager of Digital & Computational Pathology at Philips. “With digital pathology and the application of smart software, we aim to help pathologists boost efficiency, with the goal of ensuring accurate and personalized diagnoses for patients.”[163]
South Africa: Connecting Pregnant Women and New Mothers to Vital Services and Information
Source: Adapted from a case study by the Praekelt Organization[164]
In order to improve maternal health and give newborn children the best possible chance in life, pregnant women need to be provided with both timely information they can use to look after their health and access services. To truly shift health outcomes, however, national-scale systems are required. Under the leadership and stewardship of the National Department of Health and a group of committed partners, Praekelt has developed a platform that serves approximately 65 percent of women in the country.
MomConnect is a multifaceted program that creates demand for maternal health services as well as improves the supply and quality of those services. It includes stage-based health messages developed by the National Department of Health with support from project partners Baby Center, a text-based help desk that provides answers to pressing questions, a library of health information accessed via an Unstructured Supplementary Service Data menu, and a service-rating feature that allows subscribers to report on the quality of services they receive at facilities.[165] Integrating directly with the national health system, MomConnect presents decision-makers with control interfaces and dashboards to ensure feedback from mothers reaches the highest levels of government.
Over 95 percent of clinics and health facilities in the country are participating in the program, allowing over 2 million pregnant women and new mothers to become MomConnect subscribers. Aside from the sheer scale of the program, one of the most-notable achievements is the high level of engagement elicited from subscribers. Over 27 percent of them have completed service ratings, and more than half a million messages have been received and processed by the MomConnect helpdesk.
The project leaders are constantly evolving the technologies and strategies that underpin the MomConnect program. In December 2017, MomConnect was one of the first programs to pilot WhatsApp’s enterprise solution, showing impressive engagement in its rollouts. Thanks to the success of MomConnect, the Maternal Health Platform will soon be deployed in other countries, including Nigeria and Uganda, in order to improve maternal health.
South Africa: SMS to Promote Medicines Adherence
Source: Adapted from SIMpill® Medications Adherence Solution[166]
Drug adherence is a growing concern for governments, health-care systems, clinicians, and other stakeholders because of mounting evidence nonadherence is prevalent and associated with adverse health outcomes and higher costs of care. On average, 40 percent of patients enrolled in sub-Saharan African antiretroviral therapy programs discontinue their treatment after two years. Some examples of poor patient medication adherence include not taking the medication on time, in the correct doses, or at all. Reasons for not following the proper medication regimen include lack of transportation; bad weather; a worsening condition that prevents individuals from leaving home; unpleasant side effects such as confusion and forgetfulness; language barriers; and feeling “too good” to need medicine.
A number of mobile technology products have been developed to counteract these challenges. One such product is SIMpill®, a real-time drug-adherence solution that uses SMS to send messages to patients whenever they forget to take their medicine as prescribed, and alerts caregivers, family members, and friends if they continue to neglect to follow their prescriptions:
- The SIMpill® Medication Adherence System monitors patients’ medication intake and reminds them in real time whenever they forget to take the medication as prescribed. The system allows for:
- real-Time data and analysis of patients’ intake of medication;
- reminders to the patients whenever a medication event is missed;
- escalated reminder service to be available to approved key caregivers;
- warnings whenever patients take their medication at incorrect times; and
- real-time prescription management.
Using a proprietary web-based program, the monitoring system used by SIMpill® detects noncompliance in real time. Its system can escalate a timely, appropriate response to fit the needs of the patients and caregivers. The prescribed schedules trigger an SMS message sent to the patients’ phones to, for example, caution them their medication should not be taken at a later time and informing them when next to medicate. Data on levels of compliance and responses to reminders is reported to the health workers caring for the patients.
Vietnam: Modern Data Standards to Roll Out Electronic Health Records and Futureproof the Health-Care System
Vietnam, like many other developing countries, is dealing with the double burden of infectious and noncommunicable diseases. Cancer is rapidly becoming a particular problem in Vietnam, with cases tripling over the last 30 years.[167]
Effective treatment and monitoring is complicated and delayed by traditional paper patient records, which are at risk of going missing in transit, or mistakes being made. Better health information is crucial to manage more complex chronic diseases, which often require multiple specialists and a lot of patient data exchange.
A better way is to put those records online so all clinicians in the health-value chain have instant access. Online personal health records make it easier for doctors to make an early diagnosis as well as easily monitor symptoms.
For example, a diabetic patient with hypertension requires regular checkups and monitoring, often with different specialists in different locations. Data is recorded during each interaction, which needs to be accessible to all the relevant clinicians and the patients themselves. EHRs also benefit urgent interventions such as surgery, cutting treatment errors, and reducing time and bureaucracy, while facilitating insurance reimbursements.
Accordingly, the Vietnamese government in 2017 committed to spending VND5 trillion ($220 million) to create a nationwide system of electronic medical records. The plan was for 90 percent of all residents to have an electronic health record by 2025.[168] Under the plan, the government will still issue paper-based records to patients, gradually replacing them with a digital system built and run by the welfare agency Vietnam Social Security.
The Ministry of Health has been piloting software that compiles residents’ medical records into one electronic database at 26 communal medical centers in Hà Ná»™i, HCM City, Lào Cai, Yên Bái, Hà TÄ©nh, Khánh Hoà, Lâm Äồng, and Long An since June 2018.[169]
One major challenge has been the standardization of information to allow all players in the health value chain to access and record data, as well as ensuring its security. Vietnam has opted to use the HL7 Fast Healthcare Interoperability Resources framework as a practical solution for health data exchange and information systems interoperability.[170] This modern standard will allow Vietnam to futureproof its health-care system, enabling it to take advantage of the growth of the Internet of Things, the explosion of connected devices, and increases in more complex, detailed data.[171]
Middle-income countries such as Vietnam have an enormous advantage in that they do not have to build on the legacy systems of 20 years ago, and can instead build a modern system from scratch using the latest technology. Digital tools such as EHRs will play a key role, although data management and governance will also be key.
Zambia and East African Neighbors Deploy Data to Tackle Malaria
The government of Zambia has committed to ending malaria in the country by 2021 as part of achieving its Sustainable Development Goals. In 2015, Health NGO PATH and the Tableau Foundation established Visualize No Malaria (VNM), a project designed to help the Zambian Ministry of Health achieve its target by using data and analysis to drive elimination efforts.
Led by a group of data experts, PATH and Tableau have developed operational dashboards that help district health personnel understand more clearly where malaria cases are happening and how best to intervene. The tools and data created for VNM give officials across all levels of the health system the flexibility to combine data from multiple sources, analyze it, and generate insights within user-friendly dashboards. This overview of real-time epidemiological data means bed nets can be installed when needed, homes are cleared of mosquitoes during high-risk periods, and expensive medications are not left to expire on the shelf.
The data dashboard is complemented by a range of technology solutions, including location insights and satellite imagery, automated workflow for data analytics, cloud-based communication capabilities, high-speed database solutions, storage services, and expertise in enhancing the user experience.
Designed in collaboration with Zambia’s Ministry of Health, VNM now includes eight technology and services companies all working together toward the shared goal of malaria elimination.[172]
Already, improved collection and use of data has contributed to a 92 percent reduction in malaria deaths and an 88 percent reduction in malaria cases in Zambia’s Southern Province between 2014 and 2017.[173] The campaign is being expanded to neighboring regions and countries.
Acknowledgements
This report was made possible in part by generous support from Pfizer.
About the Authors
Nigel Cory is associate director, trade policy, with the Information Technology and Innovation Foundation. He previously worked as a researcher at the Sumitro Chair for Southeast Asia Studies at the Center for Strategic and International Studies. Prior to that, he worked for eight years in Australia’s Department of Foreign Affairs and Trade, which included positions working on G20 global economic and trade issues and the Doha Development Round. Cory also had diplomatic postings to Malaysia, where he worked on bilateral and regional trade, economic, and security issues; and Afghanistan, where he was the deputy director of a joint U.S./Australia provincial reconstruction team. Cory holds a master’s in public policy from Georgetown University and a bachelor’s in international business and a bachelor’s in commerce from Griffith University in Brisbane, Australia.
Philip Stevens is the executive director of the Geneva Network, which he founded in 2015. He is also a senior fellow at the Institute for Democracy and Economic Affairs, Malaysia. Formerly he was an official at the World Intellectual Property Organization (WIPO) in Geneva, where he worked in its Global Challenges Division. Philip has also worked as director of policy for International Policy Network, a United Kingdom-based think tank, as well as holding research positions with the Adam Smith Institute and Reform—both public policy think tanks in London. He holds degrees from the London School of Economics and the University of Durham, United Kingdom.
About ITIF
The Information Technology and Innovation Foundation (ITIF) is a nonprofit, nonpartisan research and educational institute focusing on the intersection of technological innovation and public policy. Recognized as the world’s leading science and technology think tank, ITIF’s mission is to formulate and promote policy solutions that accelerate innovation and boost productivity to spur growth, opportunity, and progress.
About Geneva Network
Geneva Network is a United Kingdom-based public policy research and advocacy organization working at the nexus of international intellectual property, development and trade issues which seeks to bring evidence-based analysis to debates surrounding these critical public policy issues.
For more information, visit us at www.itif.org.
Endnotes
[1]Pathways for Prosperity Commission, The Digital Roadmap: How developing countries can get ahead (Oxford: Pathways for Prosperity Commission, 2019), https://bsg-pathwaystoprosperity.s3.eu-west-2.amazonaws.com/The_Digital_Roadmap.pdf.
[2]From the ITU: E-Health refers to the use of ICTs to support health needs, while telemedicine is considered the part of eHealth wherein telecommunication systems allow the interconnection of remote locations to enable remote access to distant medical resources and expertise. In contrast, mHealth is a subset of eHealth and defined as the use of mobile wireless technologies for health. “Digital health and standards,” International Telecommunications Union website, https://www.itu.int/en/ITU-T/e-Health/Pages/default.aspx; World Health Organization, WHO guideline: recommendations on digital interventions for health system strengthening, (Geneva: WHO, 2019), https://apps.who.int/iris/bitstream/handle/10665/311941/9789241550505-eng.pdf?ua=1.
[3]The Lancet’s Global Burden of Disease report estimates that only half of all countries had the workers required to deliver good quality health care, which is estimated at 30 physicians, 100 nurses or midwives, and 5 pharmacists per 10,000 people. “The Lancet’s Global Burden of Disease,” The Lancet, accessed January 25, 2020, https://www.thelancet.com/gbd.
[4]Global Observatory for eHealth, Global Diffusion of eHealth: Making Universal Health Coverage Achievable. Report of the third global survey on eHealth (Geneva: WHO, 2016), http://apps.who.int/iris/bitstream/10665/252529/1/9789241511780-eng.pdf?ua=1.
[5]World Health Organization, WHO Guideline: recommendations on digital interventions for health system strengthening (Geneva: WHO, 2019), https://www.who.int/reproductivehealth/publications/digital-interventions-health-system-strengthening/en/; “Digital health and standards,” International Telecommunications Union website, https://www.itu.int/en/ITU-T/e-Health/Pages/default.aspx.
[6]Stephen Ezell, Mark Schultz, and David Lund, “How Innovators Are Solving Global Health Challenges” (ITIF, April 2018), /publications/2018/04/24/innovate4health-how-innovators-are-solving-global-health-challenges.
[7]Daniel Castro and Travis Korte, “Comments to the Senate Finance Committee on Health Data Transparency” (The Center for Data Innovation, August 1, 2014), http://www2.datainnovation.org/2014-senate-finance-health-data.pdf.
[8]Joshua New, “The Promise of Data-Driven Drug Development” (Center for Data Innovation, September, 2019), https://www.datainnovation.org/2019/09/the-promise-of-data-driven-drug-development/.
[9]Peter Loftus, “Drugmakers Turn to Data Mining to Avoid Expensive, Lengthy Drug Trials,” The Wall Street Journal, December 23, 2019, https://www.wsj.com/articles/drugmakers-turn-to-data-mining-to-avoid-expensive-lengthy-drug-trials-11577097000; Joshua New, “The Promise of Data-Driven Drug Development.”
[10]Mobile Ecosystem Forum, “Global mHealth & Wearables Report 2015” (MEF, 2015), https://mobileecosystemforum.com/mef-global-mhealth-and-wearables-report-2015/; PriceWaterhouseCoopers Health Research Institute, “Top Health Industry Issues of 2015” (PWC, December 2014), http://www.pwc.com/us/en/healthindustries/top-health-industry-issues/assets/pwc-hri-top-healthcare-issues-2015.pdf.
[11]Murray Aitken and Jennifer Lyle, “Patient Adoption of mHealth, Use, Evidence and Remaining Barriers to Mainstream Acceptance” (IMS Institute for Healthcare Informatics, September 2015), https://www.iqvia.com/-/media/iqvia/pdfs/institute-reports/patient-adoption-of-mhealth.pdf.
[12]PriceWaterhouseCoopers, “Emerging mHealth: Paths for Growth” (London: PWC, 2012), https://www.pwc.com/gx/en/healthcare/mhealth/assets/pwc-emerging-mhealth-full.pdf.
[13]Lee Dentith, “How Digital Healthcare Can Transform the Workplace,” Now GP blog, November 17, 2016, http://www.nowgp.com/blog/digital-healthcare-transform-workplace/.
[14]International Telecommunication Union, “Measuring the Information Society Report 2016 Key Findings” (Geneva: ITU, 2016), http://www.itu.int/en/ITU-D/Statistics/Documents/publications/misr2016/MISR2016-KeyFindings.pdf.
[15]Broadband Commission for Sustainable Development (ITU and UNESCO), “Broadband Targets for 2015” (Geneva: ITU and UNESCO 2015), https://www.broadbandcommission.org/Documents/publications/Broadband_Targets.pdf.
[16]Jiang X, Ming WK, and You JH, “The Cost-Effectiveness of Digital Health Interventions on the Management of Cardiovascular Diseases: Systematic Review,” Journal of Medical Internet Research 2019; 21(6):e13166. DOI: 10.2196/13166.
[17]“Global Digital Health Index,” Health Enabled and Global Development Incubator, accessed January 2020 https://www.digitalhealthindex.org/.
[18]Ibid.
[19]Ibid.
[20]Broadband Commission for Sustainable Development (ITU and UNESCO), Digital Health: A Call for Government Leadership and Cooperation between ICT and Health, (Geneva: ITU and UNESCO February 2017), https://www.broadbandcommission.org/Documents/publications/WorkingGroupHealthReport-2017.pdf.
[21]Ibid.
[22]World Health Organization, Global Observatory for eHealth, “Third Global Survey on eHealth, 2015,” (Geneva: WHO, 2015) http://www.who.int/goe/survey/2015survey/en/; Survey responses are the subject of rigorous attempts at standardization, but nevertheless, countries respond according to their own criteria and view of the policy situation. This means survey responses should be similar, but may not be fully consistent at the international scale.
[23]“The State of Digital Health 2019,” HealthEnabled and Global Development Incubator, accessed January 2020 https://www.digitalhealthindex.org/stateofdigitalhealth19.
[24]World Health Organization, Atlas of eHealth country profiles: The use of eHealth in support of universal health coverage, (Geneva: WHO, 2015), https://www.who.int/publications-detail/atlas-of-ehealth-country-profiles-the-use-of-ehealth-in-support-of-universal-health-coverage.
[25]Dr. Mohammad Emdadul Haque et al., “The challenges of eHealth implementation in developing countries: A literature review,” Journal of Dental and Medical Services, Volume 18, Issue 5 Ser 12 (May 2019), 41–57, https://www.iosrjournals.org/iosr-jdms/papers/Vol18-issue5/Series-12/H1805124157.pdf.
[26]Patricia Mechael and Joanne Ke Edelman, “The State of Digital Health 2019” (Washington, D.C.: HealthEnabled and Global Development Incubator, April 2019), https://static1.squarespace.com/static/5ace2d0c5cfd792078a05e5f/t/5d4dcb80a9b3640001183a34/1565379490219/State+of+Digital+Health+2019.pdf.
[27]World Health Organization, “Global Strategy on Digital Health 2020–2024” (Geneva: WHO, March 2019), https://extranet.who.int/dataform/upload/surveys/183439/files/Draft%20Global%20Strategy%20on%20Digital%20Health.pdf.
[28]Doreen Bogdan-Martin, “Measuring digital development: Facts & figures 2019,” ITU News, November 5, 2019, https://news.itu.int/measuring-digital-development-facts-figures-2019/.
[29]“Digital Health Leadership Program,” African Alliance of digital health networks, accessed January 2020, https://www.africanalliance.digital/programs-digital-health-leadership-program.
[30]Ibid.
[31]Patricia Mechael and Joanne Ke Edelman, “The State of Digital Health 2019” (Washington, D.C.: Health Enabled and Global Development Incubator, April 2019), 22, https://www.digitalhealthindex.org/stateofdigitalhealth19.
[32]Ibid.
[33]World Health Organization, “Annex 1: Action Plan for the Global Strategy on Digital Health 2020–2024.”
[34]“New ITU statistics show more than half the world is now using the Internet,” ITU News, December 6, 2018, https://news.itu.int/itu-statistics-leaving-no-one-offline/.
[35]Mobile cellular networks now cover most of the planet, with 97 percent of the global population within reach of a mobile signal, and at least 93 percent of the global population able to access 3G or higher mobile broadband services. Doreen Bogdan-Martin, “Measuring digital development: Facts & figures 2019,” ITU News, November 5, 2019, https://news.itu.int/measuring-digital-development-facts-figures-2019/.
[36] Patricia Mechael and Joanne Ke Edelman, “The State of Digital Health 2019.”
[38]Judith E. Tyson, “Private infrastructure financing in developing countries. Five challenges, five solutions” (working paper 536, Overseas Development Institute, London, August 2018), https://www.odi.org/sites/odi.org.uk/files/resource-documents/12366.pdf.
[39]“Closing the Investment Gap: How Multilateral Development Banks Can Contribute to Digital Inclusion” (Washington, D.C.: World Wide Web Foundation, April 2018), https://webfoundation.org/research/closing-the-investment-gap-how-multilateral-development-banks-can-contribute-to-digital-inclusion/.
[40]Ibid.
[41]A guaranteed market may follow a similar model to that of the advanced market commitment (AMC) mechanism for vaccines (GAVI, 2019). The launch of the AMC program in the 2000s vastly increased the market size for companies, effectively de-risking the market, and commensurately increased the reach and quality of vaccines, enabling life-saving products to reach the poorest. For more on the application of this model to digital technologies, see Digital Impact Alliance (2018).
[42]World Health Organization, Atlas of eHealth country profiles.
[43]Michael Shapiro et al., “Patient-Generated Health Data” (white paper prepared for Office of Policy and Planning, Office of the National Coordinator for Health Information Technology, RTI International, April 2012), http://www.healthit.gov/sites/default/files/rti_pghd_whitepaper_april_2012.pdf; “Patient-Generated Health Data,” Health IT.gov, http://www.healthit.gov/policy-researchers-implementers/patient-generatedhealth-data.
[44]Murray Aitken and Jennifer Lyle, “Patient Adoption of mHealth: Use, Evidence and Remaining Barriers to Mainstream Acceptance” (IMS Institute for Healthcare Informatics, September 2015), https://www.iqvia.com/-/media/iqvia/pdfs/institute-reports/patient-adoption-of-mhealth.pdf.
[45]Food and Drug Administration, “Framework for FDA’s Real-World Evidence Program,” (Washington, D.C.: U.S. FDA, December 2018), https://www.fda.gov/media/120060/download; “Real World Evidence,” Food and Drug Administration, accessed January 2020, https://www.fda.gov/science-research/science-and-research-special-topics/real-world-evidence.
[46]Pathways for Prosperity Commission, The Digital Roadmap: How developing countries can get ahead.
[47]Sara Jerving, “Data gaps threaten achievement of development goals in Africa,” DevEx News, October 15, 2019, https://www.devex.com/news/data-gaps-threaten-achievement-of-development-goals-in-africa-95825; Mo Ibrahim Foundation (MIF), Agendas 2063 & 2030: Is Africa on Track? (London: MIF, October 2019), http://mo.ibrahim.foundation/sites/default/files/2019-10/African%20Governance%20Report%202019.pdf; African Development Working Group (Center for Global Development & The African Population and Health Research Center), Delivering on the Data Revolution in Sub-Saharan Africa (Washington, D.C.: Center for Global Development & The African Population and Health Research Center, 2014), https://www.cgdev.org/sites/default/files/CGD14-01%20complete%20for%20web%200710.pdf.
[48]“Praia Group,” Praia Group on Governance Statistics, accessed January 2020 http://www.ine.cv/praiagroup/; Sara Jerving, “Data gaps threaten achievement of development goals in Africa”; Data Revolution Group, “A World That Counts: Mobilizing the Data Revolution for Sustainable Development,” (New York: UN, 2014), https://www.undatarevolution.org/wp-content/uploads/2014/11/A-World-That-Counts.pdf.
[49]Health Data Collaborative (Health Data Collaborative Secretariat), “Health Data Collaborative Progress Report 2016–18” (Geneva: HDCS, June 2018), https://www.healthdatacollaborative.org/fileadmin/uploads/hdc/Documents/HDC_Progress_Report_Update_AW_071218_Web.pdf.
[50]“Health Data Collaborative Where We Work,” Health Data Collaborative, accessed January 2020, https://www.healthdatacollaborative.org/where-we-work/.
[51]“Health Data Collaborative Tools and Guidance,” Health Data Collaborative, accessed January 2020, https://www.healthdatacollaborative.org/resources/tools-and-guidance/.
[52]Pathways for Prosperity Commission, The Digital Roadmap: How developing countries can get ahead.
[53]Daniel Castro, “The Rise of Data Poverty in America” (Center for Data Innovation, September 2014), http://www2.datainnovation.org/2014-data-poverty.pdf.
[54]Ibid.
[55]John Pescatore, “SANS Top New Attacks and Threat Report” (A SANS whitepaper, April 2019), https://www.infoblox.com/wp-content/uploads/infoblox-whitepaper-sans-top-new-attacks-and-threat-report.pdf.
[56]“Data Protection and Privacy Legislation Worldwide,” United Nations Conference on Trade and Development, accessed January 2020, https://unctad.org/en/Pages/DTL/STI_and_ICTs/ICT4D-Legislation/eCom-Data-Protection-Laws.aspx.
[57]Alan McQuinn and Daniel Castro, “Why Stronger Privacy Regulations Do Not Spur Increased Internet Use” (ITIF, July 2018), http://www2.itif.org/2018-trust-privacy.pdf.
[59]Broadband Commission for Sustainable Development (ITU and UNESCO), Digital Health: A Call for Government Leadership and Cooperation between ICT and Health..
[60]Sarah Neville, “Value from health data creates dilemma for society,” The Financial Times, October 31, 2019, https://www.ft.com/content/4b13402a-f65a-11e9-9ef3-eca8fc8f2d65.
[61]For a comprehensive assessment of all the parts of a potential privacy framework, see: Alan McQuinn and Daniel Castro, “A Grand Bargain on Data Privacy Legislation for America” (ITIF, January 14, 2019), /publications/2019/01/14/grand-bargain-data-privacy-legislation-america.
[62]Nigel Cory, Robert D. Atkinson, and Daniel Castro, “Principles and Policies for ‘Data Free Flow with Trust’” (ITIF, May 2019), /publications/2019/05/27/principles-and-policies-data-free-flow-trust.
[63]“OECD Guidelines on the Protection of Privacy and Transborder Flows of Personal Data“ (O ECD), http://www.oecd.org/document/18/0,3343,en_2649_34255_1815186_1_1_1_1,00.html;
[64]Pathways for Prosperity Commission, The Digital Roadmap: How developing countries can get ahead.
[65]“OECD Privacy Guidelines” (O ECD), accessed January 2020, https://www.oecd.org/sti/ieconomy/privacy-guidelines.htm.
[66]World Health Organization, Atlas of eHealth country profiles.
[67]Ibid.
[68]Ibid.
[69]Ibid.
[70]Ibid.
[71]Jussi Sane and Michael Edelstein, “Overcoming Barriers to Data Sharing in Public Health: A Global Perspective” (Chatam House April 2015), https://www.chathamhouse.org/sites/default/files/field/field_document/20150417OvercomingBarriersDataSharingPublicHealthSaneEdelstein.pdf; Jean-Paul Chretien, Caitlin M. Rivers, and Michael A. Johansson, “Make Data Sharing Routine to Prepare for Public Health Emergencies,”. PLOS Medicine, August 16, 2016, https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1002109; “Data Sharing during the West Africa Ebola Public Health Emergency: Case Study Report” (Georgetown University, Center for Global Health Science and Security, November 2018), https://www.glopid-r.org/wp-content/uploads/2019/07/data-sharing-during-west-africa-ebola-public-health-emergency-case-study-report-georgetown.pdf.
[72]Ben Goldacre et al., WHO consultation on Data and Results Sharing During Public Health Emergencies (Oxford: Centre for Evidence-Based Medicine, Oxford University, the United Kingdom, 2015), https://www.who.int/medicines/ebola-treatment/background_briefing_on_data_results_sharing_during_phes.pdf.
[73]“Waiting on hold,” The Economist, October 27, 2014, https://www.economist.com/science-and-technology/2014/10/27/waiting-on-hold; Ed Naef et al., Using Data for Development (Boston: Cartesian consultancy services, 2014), https://docs.gatesfoundation.org/Documents/Using%20Mobile%20Data%20for%20Development.pdf.
[74]Nathan L. Yozwiak, Stephen F. Schaffner, and Pardis C. Sabeti, “Data sharing: Make outbreak research open access,” Nature, February 25, 2015, https://www.nature.com/news/data-sharing-make-outbreak-research-open-access-1.16966; Wellcome-Department for International Development (DfID), Data Sharing in Public Health Emergencies: Anthropological and Historical Perspectives on Data Sharing during the 2014–2016 Ebola Epidemic and the 2016 Yellow Fever Epidemic (London: Wellcome-DfID joint report, November 26, 2018), https://www.glopid-r.org/wp-content/uploads/2019/07/data-sharing-in-public-health-emergencies-yellow-fever-and-ebola.pdf; Nigel Cory, “Viruses Cross Borders. To Fight Them, Countries Must Let Medical Data Flow, Too,” Innovation Files blog post, May 7, 2020, /publications/2020/05/07/viruses-cross-borders-fight-them-countries-must-let-medical-data-flow-too.
[75]“What is Open Data?” Open Knowledge Foundation, 2012, http://opendatahandbook.org/en/what-is-open-data/.
[76]John Holdren, “Increasing Access to the Results of Federally Funded Scientific Research,” Executive Office of the President Office of Science and Technology Policy, February 22, 2013, https://obamawhitehouse.archives.gov/sites/default/files/microsites/ostp/ostp_public_access_memo_2013.pdf; John Holdren, Letter on federal agencies' progress developing public research data access plans, March 24, 2014, https://obamawhitehouse.archives.gov/sites/default/files/microsites/ostp/OpenAccess_March-2014.pdf.
[77]“Comments in response to the White House Office of Science and Technology Policy Request for Information: Public Access to Peer-Reviewed Scholarly Publications Resulting From Federally Funded Research,” Mendeley, 2011, https://obamawhitehouse.archives.gov/sites/default/files/microsites/ostp/Scholarly%20Pubs%20Comments%20101-200.pdf.
[78]Jean-Paul Van Belle et al., “Africa Data Revolution Report 2018: Status and Emerging Impact of Open Data in Africa” (Geneva: World Wide Web Foundation, 2018), https://webfoundation.org/docs/2019/03/Africa-data-revolution-report.pdf; Leo Mutuku and Teg-wende Idriss Tinto, “Open Data Around the World - Sub-Saharan Africa,” State of Open Data, https://stateofopendata.od4d.net/chapters/regions/sub-saharan-africa.html.
[79]“Data Driven Development: Pathways for Progress” (Geneva: World Economic Forum, January 2015), http://www3.weforum.org/docs/WEFUSA_DataDrivenDevelopment_Report2015.pdf.
[80]African Development Working Group (Center for Global Development & The African Population and Health Research Center), “Delivering on the Data Revolution in Sub-Saharan Africa,” (Washington, D.C.: Center for Global Development & The African Population and Health Research Center, 2014), https://www.cgdev.org/sites/default/files/CGD14-01%20complete%20for%20web%200710.pdf.
[81]Ibid.
[82]As opposed to compulsory access, as advocated in the WEF report. “Many concerns about sharing data are based on a lack of trust, a fear of incurring liabilities or a loss of institutional information control and arbitrage advantages (which create and maintain power differentials both within and between organizations). Overcoming some of the issues that limit data sharing may require more direct forms of external compulsion in the form of improved oversight and enforcement, where such an authority is available (either by government regulation or enforceable stakeholder self-regulation). “Data Driven Development: Pathways for Progress.”
[83]Ibid.
[84]“Notice of Proposed Rulemaking to Improve the Interoperability of Health Information,” U.S. Department of Health and Human Services, https://www.healthit.gov/topic/laws-regulation-and-policy/notice-proposed-rulemaking-improve-interoperability-health.
[85]Damian Garde, “Big Pharma superteam joins NIH to share data, discover new drugs,” FierceBiotech, February 4, 2014, https://www.fiercebiotech.com/partnering/big-pharma-superteam-joins-nih-to-share-data-discover-new-drugs.
[86]Harlan Krumholz, “Time To Assess Pharma Progress In Data Sharing,” Forbes, June 2, 2014, https://www.forbes.com/sites/harlankrumholz/2014/06/02/time-to-assess-pharma-progress-in-data-sharing/.
[87]As has been raised in the United States and the USDA. Michael Causey, “Medical Device Makers Urged to Play Nicer by Sharing Data,” Quality Digest, February 19, 2014, https://www.qualitydigest.com/inside/fda-compliance-column/medical-device-makers-urged-play-nicer-sharing-data-021914.html.
[88] “Notice of Proposed Rulemaking to Improve the Interoperability of Health Information.”
[89]Leo Mutuku and Teg-wende Idriss Tinto, “Open Data Around the World - Sub-Saharan Africa.”
[90]Vincent D. Blondel et al., “Data for Development: The D4D Challenge on Mobile Phone Data,” arXiv, January 2013, https://arxiv.org/pdf/1210.0137.pdf
[91]“Data Collaboratives,” New York University, accessed January 2020, https://datacollaboratives.org/.
[92]Ibid.
[93]Joshua New, “The Promise of Data-Driven Drug Development.”
[94]“Blue Button,” HealthIT.gov, https://www.healthit.gov/topic/health-it-initiatives/blue-button.
[95]Nigel Cory, “Viruses Cross Borders. To Fight Them, Countries Must Let Medical Data Flow, Too,” Innovation Files blog post, May 7, 2020, /publications/2020/05/07/viruses-cross-borders-fight-them-countries-must-let-medical-data-flow-too.
[96] Nigel Cory, “Cross-Border Data Flows: Where Are the Barriers, and What Do They Cost?” (ITIF, May 2017), /publications/2017/05/01/cross-border-data-flows-where-are-barriers-and-what-do-they-cost.
[97]Personally Controlled Electronic Health Records Act 2012, no. 63, Australia (2012), https://www.legislation.gov.au/Details/C2012A00063.
[98]Anupam Chander and Uyen P. Le, “Data Nationalism,” Emory Law Journal 64, no. 3 (2015), https://ssrn.com/abstract=2577947.
[99]“Interpretation on Population Health Information Management Measures (Trial Implementation),” National Health and Family Planning Commission of the PRC, last updated June 15, 2014, http://en.nhc.gov.cn/2014-06/15/c_46801.htm; Nigel Cory, “The Worst Innovation Mercantilist Policies of 2016” (ITIF, January 2017), http://www2.itif.org/2017-worst-innovation-mercantilist-policies.pdf; Regulation on the Credit Reporting Industry, State Council 228th session, China (2013), http://www.pbccrc.org.cn/crc/jgyhfw/201309/1ca0f775b50744cabaf83538288d77a9/files/e8a8bf080ed64f48914a652da1d8fdc3.pdf.
[100]National House Ordinance of the People’s Republic of China No. 717, (2019), http://www.gov.cn/zhengce/content/2019-06/10/content_5398829.htm; David Cyranoski, “China’s crackdown on genetics breaches could deter data sharing,” Nature, November 2018, https://www.nature.com/articles/d41586-018-07222-2.
[101] Reserve Bank of India, “Frequently Asked Questions,” RBI website, https://m.rbi.org.in/Scripts/FAQView.aspx?Id=130; Surabhi Agarwal, “Govt looks to keep tabs on tech giants with data centres in India,” The Economic Times, April 14, 2018, https://economictimes.indiatimes.com/news/economy/policy/govt-looks-to-keep-tabs-on-tech-giants-with-data-centres-in-india/articleshow/63756058.cms.
[102]“Russia’s Personal Data Localization Law Goes Into Effect,” Duane Morris, October 16, 2015, http://www.duanemorris.com/alerts/russia_personal_data_localization_law_goes_into_effect_1015.html?utm_source=Mondaq&utm_medium=syndication&utm_campaign=View-Original.
[103] Hannah Kim, So Yoon Kim, and Yann Joly, “South Korea: in the midst of a privacy reform centered on data sharing,” PMC, August 18, 2018, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6132641/; Ozan Karaduman, “The New Personal Data Protection Law 2019 in Turkey,” Guen + Partners, February 14, 2019, https://gun.av.tr/the-new-personal-data-protection-law-2019-in-turkey/.
[104] Nigel Cory, “Cross-Border Data Flows: Where Are the Barriers, and What Do They Cost?”.
[105]Michelle A. Wein, Stephen J. Ezell, and Robert D. Atkinson, “The Global Mercantilist Index: A New Approach to Ranking Nations’ Trade Policies” (ITIF, October 2014), http://www2.itif.org/2014-general-mercantilist-index.pdf.
[106] Michael S. Rosenwald, “Cloud Centers Bring High-Tech Flash but Not Many Jobs to Beaten-Down Towns,” The Washington Post, November 24, 2011, http://www.washingtonpost.com/business/economy/cloud-centersbring-high-tech-flash-but-not-many-jobs-to-beaten-down-towns/2011/11/08/gIQAccTQtN_story.html; Henry Blodget, “The Country’s Problem in a Nutshell: Apple’s Huge New Data Center in North Carolina Created Only 50 Jobs,” Business Insider, November 28, 2011, http://www.businessinsider.com/apple-new-data-center-north-carolina-created-50-jobs-2011-11; Darrell Etherington, “Apple to Build a $2 Billion Data Command Center in Arizona,” TechCrunch, February 2, 2015, https://techcrunch.com/2015/02/02/apple-to-build-a-2-billion-data-command-center-in-arizona/; Rich Miller, “The Economics of Data Center Staffing,” Data Center Knowledge, January 18, 2008, http://www.datacenterknowledge.com/archives/2008/01/18/the-economics-of-data-center-staffing/; Alison DeNisco Rayome, “Why data centers fail to bring new jobs to small towns,” TechRepublic, September 19, 2016, https://www.techrepublic.com/article/why-data-centers-fail-to-bring-new-jobs-to-small-towns/.
[107] Grant Gross, “This Wave of Data Center Consolidation is Different from the First One,” Data Center Knowledge, February 8, 2018, https://www.datacenterknowledge.com/manage/wave-data-center-consolidation-different-first-one.
[108]Nigel Cory, “Cross-Border Data Flows: Where Are the Barriers, and What Do They Cost?”
[109]Bruce Japsen, “In India, IBM’s Watson Will Aid Cancer Care Where Doctors Are Scarce,” Forbes, December 2, 2015, http://www.forbes.com/sites/brucejapsen/2015/12/02/in-india-ibms-watson-will-aid-cancer-care-where-doctors-are-scarce/#7897ca1c4ff9; Matthew Wall, “How Drug Development Is Speeding Up in the Cloud,” BBC, February 21, 2017, http://www.bbc.com/news/business-39026239; William Vorhies, “Big Data in Medicine—Evolution and Revolution,” Data Science Central, November 23, 2015, http://www.datasciencecentral.com/profiles/blogs/big-data-in-medicine-evolution-and-revolution.
[110] Nigel Cory, “Viruses Cross Borders. To Fight Them, Countries Must Let Medical Data Flow, Too.”
[111] Joshua New, “The Promise of Data-Driven Drug Development.”.
[112] Moritz Lehne et al., “Why digital medicine depends on interoperability,” NPJ Digit Medicine, 2019;2:79. DOI: https://doi.org/10.1038/s41746-019-0158-1.
[113] World Health Organization, Atlas of eHealth country profiles.
[114] Pathways for Prosperity Commission, The Digital Roadmap: How developing countries can get ahead; Pathways for Prosperity Commission, “Forthcoming: Digital technology governance: developing country priorities and concerns,” accessed January 2020 https://pathwayscommission.bsg.ox.ac.uk/Digital-technology-governance.
[115] Eline Chivot and Nigel Cory, “Response to European Commission Consultation on Transfers of Personal Data to Third Countries and Cooperation Between Data Protection Authorities” (The Information Technology and Innovation Foundation, April 29, 2020), /publications/2020/04/29/response-european-commission-consultation-transfers-personal-data-third.
[116] “Organisation for Economic Cooperation and Development Privacy Guidelines,” OECD website, https://www.oecd.org/sti/ieconomy/privacy-guidelines.htm.
[117] “The Case for Accountability: How it Enables Effective Data Protection and Trust in the Digital Society” (Center for Information Policy Leadership, July 23, 2018), https://www.informationpolicycentre.com/uploads/5/7/1/0/57104281/cipl_accountability_paper_1_-_the_case_for_accountability_-_how_it_enables_effective_data_protection_and_trust_in_the_digital_society.pdf.
[118] “The APEC Cross-Border Privacy Rules (CBPR) System,” Cross Border Privacy Rules System, accessed March 21, 2019, http://cbprs.org/.
[119] “APEC Privacy Framework (2005),” Asia-Pacific Economic Cooperation, accessed March 21, 2019, https://www.apec.org/Publications/2005/12/APEC-Privacy-Framework; “APEC Privacy Framework (2015),” Asia-Pacific Economic Cooperation, accessed March 21, 2019, https://www.apec.org/Publications/2017/08/APEC-Privacy-Framework-(2015).
[120] “FTC Approves Final Orders Resolving Allegations That Companies Misrepresented Participation in International Privacy Program,” U.S. Federal Trade Commission, accessed March 21, 2019, https://www.ftc.gov/news-events/press-releases/2017/04/ftc-approves-final-orders-resolving-allegations-companies?utm_source=govdelivery.
[121] Pathways for Prosperity Commission, The Digital Roadmap: How developing countries can get ahead.
[122] “Joint statement on e-commerce news archives”, World Trade Organization (WTO), accessed January 2020, https://www.wto.org/english/news_e/archive_e/jsec_arc_e.htm.
[123] Craig Timberg, Elizabeth Dwoskin, Drew Harwell, and Tony Romm, “Governments around the world are trying a new weapon against coronavirus: Your smartphone,” Washington Post, April 17, 2020, https://www.washingtonpost.com/technology/2020/04/17/governments-around-world-are-trying-new-weapon-against-coronavirus-your-smartphone/.
[124] World Health Organization (WHO), “Global Strategy on Digital Health 2020–2024.”
[125] “WHO expert panel on digital health meets for first time,” World Health Organization news release, October 25, 2019, https://www.who.int/news-room/detail/25-10-2019-who-expert-panel-on-digital-health-meets-for-first-time.
[126] “Digital technology for COVID-19 response,” World Health Organization news release, April 3, 2020, https://www.who.int/news-room/detail/03-04-2020-digital-technology-for-covid-19-response.
[127] “Global Digital Health Partnership,” Global Digital Health Partnership, https://www.gdhp.org/.
[128] “The Principles of Donor Alignment for Digital Health,” Digital Investment Principles, https://digitalinvestmentprinciples.org/.
[129] UNICEF Health Section Implementation Research and Delivery Science Unit and the Office of Innovation Global Innovation Center, “UNICEF’s Approach to Digital Health” (New York: UNICEF, October, 2018), https://www.unicef.org/innovation/reports/unicefs-approach-digital-health%E2%80%8B%E2%80%8B.
[130] Broadband Commission for Sustainable Development (ITU and UNESCO), Digital Health: A Call for Government Leadership and Cooperation between ICT and Health.
[131] Broadband Commission for Sustainable Development (ITU and UNESCO), Working Group on Digital Health: The Promise of Digital Health: Addressing Non-communicable Diseases to Accelerate Universal Health Coverage in LMICs, (Geneva: ITU and UNESCO, September 2018), https://broadbandcommission.org/Documents/publications/DigitalHealthReport2018.pdf.
[132] Pathways for Prosperity Commission, The Digital Roadmap: How developing countries can get ahead.
[133] Ibid.
[134] “Portal Telemedicina resorts to Google Cloud to offer a remote diagnosis platform,” Google Cloud case study, https://cloud.google.com/customers/portal-telemedicina/.
[135] Laurie Chen, “AI may help speed up drugs development and could have ‘immense’ impact in China, study finds,” South China Morning Post, September 3, 2019, https://www.scmp.com/news/china/science/article/3025553/ai-may-help-speed-drugs-development-and-could-have-immense.
[136] Robert D. Atkinson, “China’s Biopharmaceutical Strategy: Challenge or Complement to U.S. Industry Competitiveness?” (ITIF, August 2019), /publications/2019/08/12/chinas-biopharmaceutical-strategy-challenge-or-complement-us-industry.
[137] Daniel Castro, Michael McLaughlin, and Eline Chivot, “Who Is Winning the AI Race: China, the EU or the United States?” (ITIF, August 2019), /publications/2019/08/19/who-winning-ai-race-china-eu-or-united-states.
[138] Laurie Chen, “AI may help speed up drugs development and could have ‘immense’ impact in China, study finds.”
[139] “China investing heavily in AI to boost pharma sector, says analyst,” The Pharma Letter, October 14, 2019, https://www.thepharmaletter.com/article/china-investing-heavily-in-ai-to-boost-pharma-sector-says-analyst.
[140] Conor Hale, “Insilico signs $200m AI drug discovery partnership with China’s CTFH,” Fierce Biotech, October 9, 2019, https://www.fiercebiotech.com/medtech/insilico-signs-200m-ai-drug-discovery-partnership-china-s-ctfh.
[141] “AstraZeneca announces three large scale initiatives in China to advance global medicine research and development,” AstraZenca, November 6, 2019, https://www.astrazeneca.com/media-centre/press-releases/2019/astrazeneca-announces-three-large-scale-initiatives-in-china-to-advance-global-medicine-research-and-development-061120119.html.
[142] Shibu Vijayan, “Finding the missing millions: the importance of private sector engagement for eliminating tuberculosis,” PATH website, January 16, 2019, https://www.path.org/articles/finding-missing-millions-importance-private-sector-engagement-eliminating-tuberculosis/.
[143] “Public Private Interface Agency: Accelerating TB Elimination in India Through Private Sector Engagement,” PATH, https://path.azureedge.net/media/documents/PPIA_case_study_FINALv2_C74DlGL.pdf.
[144] Dhruv Gupta, “Increasing private practitioner engagement with tuberculosis,” Brookings blog post, October 12, 2018, https://www.brookings.edu/events/development-seminar-engaging-private-practitioners-to-improve-tuberculosis-diagnosis-and-treatment-in-urban-india/.
[145] “Mumbai Mission for TB Control, India,” Stop TB Partnership, 2014, http://www.stoptb.org/news/stories/2014/ns14_084.asp.
[146] “Physicians battle India’s diabetic retinopathy crisis”, Ocular Surgery News India Edition, July 2007, https://www.healio.com/ophthalmology/cataract-surgery/news/print/ocular-surgery-news-india-edition/%7Bf2a236c2-14d9-43e6-82c8-85acd5e96ce7%7D/physicians-battle-indias-diabetic-retinopathy-crisis.
[147] GVS Murthy and Taraprasad Das, “Diabetic care initiatives to prevent blindness from diabetic retinopathy in India,” PMC, January 2016, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4821122/.
[148] “Google teams up with Indian doctors to use AI to help diabetes patients in India”, India Today, July 11, 2019, https://www.indiatoday.in/technology/news/story/google-teams-up-with-indian-doctors-to-use-ai-to-help-diabetes-patients-in-india-1566874-2019-07-11.
[149] “Eyecare and diabetic Retinopathy: how virtual ophthalmologists can emerge a gamechanger,” Financial Express, November 4, 2019, https://www.financialexpress.com/lifestyle/health/eyecare-and-diabetic-retinopathy-how-virtual-ophthalmologists-can-emerge-a-game-changer/1753846/.
[150] “Exploring Indonesia’s healthcare startup scene,” Techcollectivesea website, December 20, 2018, https://techcollectivesea.com/2018/12/20/exploring-indonesias-healthcare-startup-scene/.
[151] “Beyond the hospital: Challenges and opportunities in Indonesian healthtech scene,”e27.co, July 9, 2019, https://e27.co/beyond-hospitals-challenges-opportunities-indonesian-healthtech-scene-20170830/
[153] “This Indonesian start-up has become the Gates Foundation’s first health care tech investment,” South China Morning Post, July 26, 2019, https://www.scmp.com/tech/start-ups/article/3020118/indonesian-start-has-become-gates-foundations-first-health-care-tech.
[154] “Life Expectancy at Birth, Total Years,” The World Bank, https://data.worldbank.org/topic/health.
[155] “Telehealth apps rise in Southeast Asia due to doctor scarcity”, Nikkei Asia Review, September 11, 2018, https://asia.nikkei.com/Business/Business-trends/Telehealth-apps-rise-in-Southeast-Asia-due-to-doctor-scarcity.
[156] Shara Senior, “Monitoring pregnancies using mobile solutions,” Philips website, https://www.philips.com/a-w/about/news/archive/blogs/innovation-matters/Monitoring_pregnancies_using_mobile_solutions.html.
[157] Human Resources for Health Strategic Plan 2011–2016, Ministry of Health Rwanda, https://medicine.yale.edu/intmed/globalhealthscholars/Images/HRH%20Strategic%20Plan%20March%202011_tcm323-158432.pdf.
[158] Number of mobile cellular subscriptions per 100 inhabitants in Rwanda from 2000 to 2018, available at https://www.statista.com/statistics/510562/mobile-cellular-subscriptions-per-100-inhabitants-in-rwanda/.
[159] Lia Novotny, “3-minute case study: The doctor will chatbot you now,” AthenaInsight.com, June 20, 2018, https://www.athenahealth.com/insight/sites/insight/files/3-minute%20case%20study%20The%20doctor%20will%20chatbot%20you%20now.pdf.
[160] Hannah Crouch, “Babylon expands its AI technology to mainland China,” Digital Health, April 10, 2018, https://www.digitalhealth.net/2018/04/babylon-ai-technology-china-tencent/.
[161] “Saudi Arabia steadily moving to build digital health ecosystem,” Saudi Gazette, November 4, 2019, http://saudigazette.com.sa/article/581708
[162] Saudi Health Council, Cancer Incidence Report Saudi Arabia 2014 (Kingdom of Saudi Arabia: Saudi Health Council, September 2017), https://nhic.gov.sa/eServices/Documents/2014.pdf.
[163] “Philips teams up with AI Borg Laboratories to help reduce the time to diagnosis for cancer patients in Saudi Arabia,” Philips News Blog, October 10, 2018, https://www.philips.co.uk/healthcare/sites/pathology/release-press/20181010-philips-teams-up-with-al-borg-laboratories-to-help-reduce-the-time-to-diagnosis-for-cancer-patients-in-saudi-arabia.
[164] “Mom Connect South Africa,” Praekelt.org, https://www.praekelt.org/momconnect.
[165] “Baby Center”, Baby Center, https://www.babycenter.com/.
[166] “SIMpill Medication Adherences Solution,” africanstrategies4heatlh.org, http://www.africanstrategies4health.org/uploads/1/3/5/3/13538666/simpill_medication_adherences_solution.pdf.
[167] Pham T et al., “Cancers in Vietnam-Burden and Control Efforts: A Narrative Scoping Review,” NCBI, 2019, Cancers in Vietnam-Burden and Control Efforts: A Narrative Scoping Review.
[168] Dean Koh, “Vietnam to deploy EHR nationwide in July”, Healthcare IT News, June 24, 2019, https://www.healthcareitnews.com/news/asia-pacific/vietnam-deploy-ehr-nationwide-july.
[169] “Citizens to have Electronic Health Records by the end of this year” Vietnam News, June 8, 2019, https://vietnamnews.vn/society/521049/citizens-to-have-electronic-medical-records-by-the-end-of-this-year.html.
[170] HL7 FHIR Release 4, available at http://www.hl7.org/fhir/?ref=learnmore.
[171] Susann Roth, “Creating Viet Nam’s digital health web,” Asian Development Bank Blog, December 2017, https://blogs.adb.org/blog/creating-viet-nam-s-digital-health-web.
[172] Jeff Benson, “It helps to have friends in tech (unless you’re a malaria parasite),” Path, April 17, 2018, https://www.path.org/articles/it-helps-to-have-friends-in-tech/.
[173] Hannah Judge, “Visualize No Malaria wins Geospatial World Excellence Award,” Mapbox Blog, April 4, 2019, https://blog.mapbox.com/visualize-no-malaria-wins-geospatial-world-excellence-award-4ec81a662f7.

