AR/VR’s Potential in Health Care
AR/VR innovation needs to accelerate in order to meet the critical demands of health care. Policymakers should empower and fund immersive technologies in the health-care industry because of the long-term cost saving benefits and positive impact on patient care.
KEY TAKEAWAYS
Key Takeaways
Contents
Value of AR/VR in Health care. 3
Who Is Using AR/VR In Health Care. 4
Barriers and Risks to Adoption. 20
Introduction
While augmented and virtual reality (AR/VR)—or extended reality (XR) more broadly—is popularly known for gaming applications, health care is quickly becoming the largest use case for these technologies. Doctors, surgeons, and medical students are not the only ones using XR for health care, either, as immersive environments can also put personal health technology in the hands of everyday consumers. In both practitioners’ and patients’ hands, medical XR (MXR) has the potential to ease some common burdens in the health-care industry, such as low health-care worker morale and retention, care deserts where a specialist is not locally available, and possibly even overreliance on opioids for pain treatment.[1]
The tremendous benefits of AR/VR for health care have driven demand, while advances in technology have driven innovation. For example, advances in artificial intelligence (AI) have become a catalyst for advances in AR/VR, as integrations with AI tools such as chatbots and data collection tools play a large role across many aspects of medicine, from diagnosis to treatment to personalized health applications. In addition, AR/VR combined with 3D modeling technology allows doctors to practice surgical simulations, teach students about anatomy, and provide patient-specific diagnoses on virtual humans and digital “twins” of existing patients.[2] These highly detailed anatomical models move beyond traditional education and medical tools, offering novel opportunities to innovate in procedures and treatments with minimal risk and improved outcomes.
Now that AR/VR has begun to demonstrate clinical utility, the health-care industry—and particularly U.S. companies—stands well poised to alter the public health system, leading to better health outcomes for all Americans. The convergence of medical necessity, technological capability, and economic opportunity creates the perfect window for AR/VR innovation. However, without policymakers’ support, the United States risks forfeiting long-term health-care cost savings, its competitive edge in the global AR/VR market, health-care accessibility, and better patient health outcomes due to overly complex regulatory pipelines and a lack of funding and research for immersive technologies.
Now that AR/VR has begun to demonstrable clinical utility, the health-care industry—and particularly U.S. companies—stands well poised to alter the public health system, leading to better health outcomes for all Americans.
This report explores the current state and potential contributions of AR/VR in health care and highlights some of the use cases currently building the foundation for immersive care. It is part of a series on AR/VR’s impact on health care, with a forthcoming report detailing AR/VR’s potential in mental health care.
Policymakers can play a valuable role in accelerating adoption and encouraging innovation of immersive technologies in health care. The report’s recommendations include:
▪ supporting federal privacy legislation to create consistent protection of AR/VR data,
▪ promoting public-private partnerships to advance AR/VR health-care innovation,
▪ increasing integration of AR/VR in health-care education and workforce development programs,
▪ improving Food and Drug Administration (FDA) approval process for AR/VR technologies,
▪ ensuring AR/VR technologies are included in Medicare and Medicaid coverage,
▪ continuing to develop standards, and
▪ continuing to fund research into immersive technologies’ impact on public health.
Value of AR/VR in Health care
The health-care industry has been exploring the potential of immersive technologies since the early 1990s, when surgical training simulators became the first successful commercial application of VR.[3] Though AR/VR gaming is currently the largest force driving the adoption of immersive technologies, for decades, health-care applications have rivaled gaming for greatest economic impact in the industry.[4] In fact, the market for AR/VR health care is expected to grow over 10 times in less than a decade, from about $4 billion in 2024 to over $46 billion by 2032.[5] Practitioners already see the potential: according to one XR Association survey, 84 percent of health-care professionals believe AR/VR will positively change the industry.[6]
Immersive technologies enhance traditional methods of health care and present new treatments to explore. For example, interactive visualizations provide precise 3D models of patients’ anatomy that can help doctors identify and understand problems more effectively than with 2D images. This allows doctors to more effectively and holistically personalize care, track treatment, and make diagnoses.
Though AR/VR gaming is currently the largest force driving the adoption of immersive technologies, for decades, health-care applications have rivaled gaming for greatest economic impact in the industry.
Additionally, AR/VR is already playing a large role in medical education.[7] Medical students increasingly rely on immersive technologies to learn and practice procedures in a risk-free, highly customizable virtual environment using specific patient information and a variety of emergency settings. In addition to helping students learn how to diagnose and treat patients, some applications can help train doctors to better empathize with patients from diverse backgrounds with different needs and react to stressful and emergent situations.
Patients will also benefit from AR/VR health-care applications. Wearables—electronic devices worn on the body, such as a smartwatch, and equipped with sensors such as heart rate monitors, glucose measuring tools, calorie intake monitors, and sleep monitors—are revolutionizing the health-care industry by allowing patients to personally track health markers without needing to get testing from medical centers. And AR/VR headsets can transform treatments and fitness activities by bringing classes and treatments into the home instead of having to travel to a medical center or gym. The likely shift away from full AR/VR headsets to lighter and more portable smart glasses may further accelerate the integration of traditional health-care treatments into users’ homes.
However, there is still much to learn about the long-term impacts of AR/VR in health care. Limited data exists on how AR/VR technologies perform compared to traditional methods. These technologies also pose novel risks, such as the higher level of distraction immersive experiences present over other technologies, the increased amount of sensitive data collection certain applications require, and the potential psychological and sensory load impacts of extended use.[8]
Who Is Using AR/VR In Health Care
Doctors and Practitioners
Immersive technologies empower doctors to be more accurate, patient centered, and efficient in a health-care landscape with more patients than ever, including in difficult-to-access rural locations, and in the face of a growing demand for personalized treatment. By enabling remote consultations, precise surgical planning through 3D modeling, and immersive training, AR/VR technologies bridge gaps in accessibility and expertise, revolutionizing how practitioners deliver care.
Day to day, doctors process large amounts of data about each patient, including information about past care. Historically, doctors have relied mostly on conversations with each patient. Now biomedical laboratories and electronic health records (EHRs) collect and store volumes of data that medical offices can more easily share with one another.[9] Not only does this data need to be as accurate as possible, but also doctors must process and make decisions on it quickly to ensure the best outcomes for their patients.
Diagnoses
Providing an accurate diagnosis is a crucial yet difficult part of health-care practitioners’ jobs. There are multiple obstacles preventing accurate diagnoses in certain cases, such as doctors needing a patient’s full medical background, high patient loads and limited consultation time, and the complexity of accurately identifying exact medical conditions. AR/VR has the potential to assist doctors in making accurate diagnoses through enhanced medical imaging and visualizations and better global collaboration with other specialists. A wide range of practitioners can benefit from using AR/VR to better make diagnoses, including dermatologists identifying skin conditions, cardiologists finding structural issues within the heart, and oncologists visualizing tumors more accurately to help treat cancer.[10]
Doctors typically look at X-rays as flat, 2D images, but the rise of 3D medical imaging means doctors can examine anatomy in more immersive ways, improving visualization of patients’ specific anatomy. AR improves medical imaging even beyond 3D images by allowing doctors to essentially have X-ray vision, allowing images of a patient’s anatomy to be overlaid directly onto the patient’s body. Between computed tomography (CT) and magnetic resonance imaging (MRI) scans, which have existed for decades, and these newer AR overlays, doctors can more accurately pinpoint what a patient’s diagnosis looks like and where exactly it is in the body.[11] By reducing diagnostic errors and better identifying patient issues, diseases could be detected earlier and doctors could provide more effective treatment.
Beyond 3D images, digital twins—digital models of physical objects, locations, and living organisms—allow doctors to create highly customized digital replicas of their patients in order to provide the most specific models of patients’ particular anatomy.[12] Digital twins require a combination of Internet-connected devices, XR technology, cloud computing, and AI all working together to create the model, capture the inputs, and store the data.[13] As a result, digital twins’ “holistic view of the patient allows for personalized treatment plans, considering individual characteristics, medical history, and real-time physiological data … With digital twins, healthcare professionals can make accurate diagnoses, monitor patients in real-time, and empower patients to actively participate in their own care.”[14]
Preparation
For surgical applications, virtual models with AR/VR can be used for planning and prepping a procedure, providing preoperative visualization for the surgical team as well as patient education. For example, head-mounted displays (HMDs) are used to show virtual medical images and patient-specific anatomical models that practitioners can manipulate and annotate ahead of procedures.[15] In addition, HMDs can assist doctors in preparing for potential challenges that may arise during surgery based on a patient’s specific history and anatomy. The technology also allows doctors to refine their technique and approach before entering a high-stress surgical setting. For patients, doctors can use these images to better explain complicated procedures by showing and illustrating a surgery, rather than trying to explain it verbally.
AR/VR can also be used for intraoperative navigation in which surgeons use real-time 3D images of a patient’s anatomy during surgery to accurately identify and target precise areas.[16] When surgeons need to constantly consult images in the operating room, they are temporarily turning and looking away from the patient. With AR/VR, the surgical team can save time and avoid distraction, since they do not need to refer to a flat screen. This reduces the mental load on surgeons, which is critical when dealing with time-sensitive procedures.[17] One study of 28 spinal surgeries finds that the AR procedure placed screws with such accuracy that the surgeons scored 98 percent on standard performance metrics, when “clinically acceptable” rates are typically around 90 percent.[18]
In addition, the ability of a team of doctors to discuss and work on specific surgical cases together via VR—without physical location limitations—means doctors across specialties around the world can support patients together, providing the most collaborative and inclusive care possible for the most difficult surgical procedures. For example, in 2023, Dr. Noor ul Owase Jeelani operated for 27 hours to successfully separate conjoined twins using XR for presurgical planning in London after consulting with specialists in Rio de Janeiro.[19] In addition, the Living Brain project crowdsources 3D brain maps to allow for better collaboration globally to improve surgical interventions for epilepsy.[20]
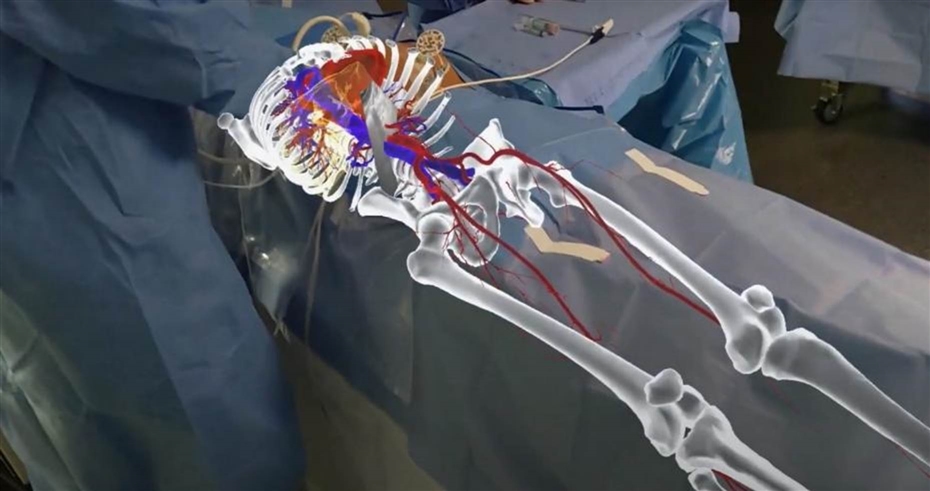
Use Case: MediView’s Surgical Live Imaging
MediView XR is a U.S.-based med-tech company specializing in the health AR ecosystem. Its XR90 platform uses mixed reality to effectively give doctors X-ray vision, enabling them to visualize vital organs inside a patient’s body during live procedures. Rather than having to consult 2D X-rays or pictures of a patient, doctors can “see” organs, bones, and skin tissue in real time as MediView’s technology mixes CT scans and live ultrasound to provide the most accurate visualizations. These visualizations are then used during minimally invasive procedures, such as skin biopses.[21] Doctors can customize the display’s placement, size, angle, and orientation to suit their unique needs.
In July 2023, the XR90 system was the first AR platform to earn FDA clearance for live imaging during medical procedures.
Figure 1: MediView XR’s holographic heads-up display[22]
Treatment and Care
According to the FDA, AR/VR devices may help increase patient compliance and adherence to therapy when it comes to pain management.[23] The technology provides a distraction technique to help manage pain, discomfort, and anxiety for patients undergoing medical and dental procedures.
For example, one study placed patients in immersive ocean and operatic settings to test if these relaxing experiences had an impact on their perception of pain via a heat experiment. The study finds that the immersive VR experience increased heat-pain tolerance, improved mood, and decreased anxiety better than the participants using nonimmersive control experiences.[24] Another study shows that patients undergoing chemotherapy for cancer had an altered perception of how much time had passed during treatment when using VR as a distraction technique, believing that the treatment session went by faster than it really did.[25]
There are promising results for this type of VR treatment for chronic pain conditions such as fibromyalgia and phantom limb pain, as well as regional pain conditions caused by injury or illness.[26] The “Snow World” application, for example, uses this distraction technique to place patients undergoing burn wound debridement in an immersive ice experience. Typically, patients rate their pain level when undergoing burn wound treatment as “severe to excruciating.” But when using the VR application, over half the patients switched their pain rating from “severe” to “mild.”[27] Though these technologies are promising for treating chronic and severe pain, more research is necessary to determine how effective these treatments are over a longer duration, and how central these interventions are to long-term pain management.
Use Case: Applied VR’s Pain Management
RelieVRx is the first FDA-authorized in-home VR treatment for chronic lower back pain. Applied VR, RelieVRx’s parent company, has a partnership with Cedars-Sinai hospital in Los Angeles, California, which is consistently ranked one of the top-performing hospitals in the United States. Cedars-Sinai also has one of the largest academic medical initiatives working on MXR.[28] Applied VR has also done research with the Cleveland Clinic, the National Cancer Institute, and the National Institute on Drug Abuse at the National Institutes of Health (NIH).[29]
The RelieVRx application uses a series of pain management techniques, including cognitive behavioral therapy, distraction, and behavior modification. Patients use the application at home over the course of 56 sessions that last only six minutes. These sessions include “mindful escapes” such as swimming with dolphins underwater, interactive games and activities, and voice-guided lessons that teach a patient how their body responds to pain. With its application, RelieVRx has found that patients experience an over 50 percent reduction in pain.[30]
Experts have seen these sorts of techniques—such as diaphragmatic breathing and distraction—help manage the body’s response to pain even before their incorporation into AR/VR technologies; however, the immersiveness of AR/VR can help transport patients to a relaxing environment while they learn, calming the nervous system in multiple ways.[31]
Figure 2: Still of Applied VR’s pain management application, teaching diaphragmatic breathing to help control patients’ nervous system responses[32]

Use Case: Smileyscope’s Pain Distraction for Kids
Smileyscope is a VR application for kids that has been proven to lessen the pain of drawing blood or intravenous (IV) insertion. The application uses a variety of virtual experiences as a pain distraction technique, in addition to incorporating music therapy into the experiences. It has been cleared for patients as young as four years old and is the first VR device to receive an FDA Class II classification.[33]
The metaverse is not designed for young people, per se, yet they are the technologies’ main adopters. This enthusiasm—and their already overwhelming use of immersive gaming apps—indicates that kids will drive the market for AR/VR technologies more broadly; immersive technologies foster social connection and stimulate creativity and imagination. Play, imagination, and creativity are all imperative for children’s development.[34]
Unfortunately, children can face physically demanding experiences in AR/VR spaces, which may lead to eye strain, fatigue, cybersickness, radiation, and sleep disorders. Children may also be more susceptible to neck strain from the weight of using a headset.Therefore, this area needs further research on long-term impacts, particularly in areas such as visual development, especially for children with cerebral palsy or Down syndrome, who may be more susceptible to already weak eye movement or control. In addition, the risks and long-term effects of AR/VR on children are mostly unknown and still being studied.[35]
Figure 3: Smileyscope pain management application, wherein users can swim with sea lions[36]

Furthermore, AR/VR may provide new and improved avenues for telemedicine. While videoconferencing appointments today allow patients to meet with their doctor without having to physically travel to see them, AR/VR can allow patients to feel like their doctor is in the room with them, leading to highly realistic appointments. This is especially important for rural areas, as patients may have to travel long distances to see their doctor; rural Americans live an average of about 10 miles from the nearest hospital, whereas suburban and urban Americans live an average of about 5 miles away.[37] This applies globally as well, as the International Labor Organization has found that 56 percent of people living in rural areas worldwide do not have access to essential health-care services, compared with 22 percent in urban areas.[38] AR/VR is also useful for military doctors, allowing them to provide guidance and advice safely to medics in warzones and other unsafe regions.[39]
It is important to note that AR/VR treatments are not useful for all patients. Many headsets’ user safety guides suggest that pregnant people, the elderly, and those who have pre-existing conditions such as epilepsy or heart conditions refrain from using the devices. Some suggest that if individuals are overly tired or suffering from a cold, headache, or upset stomach, they should avoid use because the virtual experience may worsen those conditions. Hospitals and care centers should also be cognizant of effectively sanitizing devices in between shared patient use, as the devices could spread contagious diseases or cause skin irritation in some cases.[40]
Rehabilitation
VR rehabilitation for physical and occupational therapy includes helping patients retrain motor functions, practice coordination, and simulate real-world tasks. The technology can allow patients to practice or relearn basic activities crucial to daily life, such as walking or opening doors, in a safe environment before trying the same techniques in the physical world.[41] In addition, through the gamification of physical therapy, doctors see increases in patient compliance, as traditional rehabilitation methods often fail to engage long-term patients, such as those who remain bedbound for extended periods. This approach makes physical therapy both an effective treatment and also entertaining, as well as motivates patients to stick with their therapy regimen.[42] For example, HTC Vive’s Ultimate Tracker combines a wearable with a headset and uses full-body tracking that targets specific parts of the body for personalized and focused rehab.[43] The Virtualis PhysioVR, developed with physical and occupational therapists, uses this technology in sports medicine and to address orthopedic concerns, concussions, chronic pain, and neurological issues.[44] According to XR Health, physical rehabilitation patients see a 37 percent reduction in their symptoms after 90 days.[45] This technology also allows for greater remote patient monitoring so doctors do not have to ask patients to travel for continued care, and for asynchronous interactions so doctors and patients alike are not constrained by conflicting schedules.[46]
There is also great potential for using AR/VR for rehabilitation following traumatic brain injuries and neurodegenerative diseases. For example, for those with Parkinson’s—a chronic, progressive brain disorder affecting the nervous system—VR is showing hopeful results as a more effective therapy over traditional methods because a VR environment allows patients to practice cognitive and motor activities and simulate risky activities in a safe, regulated environment.[47]
While researchers and developers are still studying AR/VR applications for communication disorders such as stuttering and voice disorders, one study suggests that the technology offers benefits over conventional assessment and treatment methods, including “the ability to manipulate task complexity and assess communication in real-world situations.”[48] The study also adds that VR may help reduce feelings of stress or embarrassment that people with communication disorders may experience in real-world conversations, creating a safer and more stable environment for practicing communication.[49]
Mental Health Practitioners
AR/VR shows a lot of promise in the field of behavioral medicine for those with autism, post-traumatic stress disorder (PTSD), attention deficit hyperactivity disorder (ADHD), substance abuse disorders, schizophrenia, depression, and other mental health disorders that require therapeutic interventions. The technology can improve medication adherence, motivation, and rehabilitation.[50] There is a growing body of evidence that VR has the potential to alleviate addiction, which could help address the opioid epidemic in the United States.[51]
AR/VR has the potential to assist doctors in making accurate diagnoses through enhanced medical imaging and visualizations and better global collaboration with other specialists.
Diagnoses
A diagnosis of mental illness is rarely simple and straightforward. There are no infallible physiological tests that determine whether a person has a specific mental illness, and doctors must often consider several symptoms in order to make as accurate a diagnosis as possible.[52] With doctors needing a full picture of a patient’s background, including potentially traumatic experiences, in addition to doctors’ limited assessment time, it can be difficult to pinpoint an exact diagnosis for a patient. One Ethiopian study suggests that more than one-third of patients with a severe psychiatric disorder have been misdiagnosed, with the most misdiagnosed condition being schizoaffective disorder at 75 percent of cases.[53] Another study from Canada suggests that misdiagnosis rates for social anxiety disorder have reached over 97 percent.[54] While research on misdiagnosis rates and identification methods for mental health disorders continues, AR/VR technology shows promise in helping doctors make more accurate diagnoses by visualizing the brain through integrated medical imaging, patient data, and AI analysis of brain activity.[55] Doctors can also create certain VR experiences to test out patients’ reaction to stimuli. However, further research is still needed to fully understand how effective AR/VR is in making accurate mental health diagnoses.
Treatment
AR/VR is a powerful tool for therapeutic interventions, offering innovative approaches to mental health care. “VR can be used to create controlled environments in which patients are guided through social situations to improve social functioning and life skills, or to design avatars, voices, and settings that approximate their perceptual disturbances to practice coping and management strategies, guided by a therapist.”[56] For instance, one method for overcoming phobias is through exposure therapy, a cognitive behavioral method wherein patients are confronted with a specific fear in a safe environment. VR can accomplish this with simulations, such as a VR simulation of crossing a high bridge for those with a fear of heights. Using AR/VR as a new therapy augmenting antipsychotic medication has shown to help improve symptoms the medication cannot treat, such as social withdrawal, functional deficits, and deficits in attention or working memory.[57]
The root causes of addiction and substance abuse disorders are still not fully understood, and like many other mental health disorders, there are few objective symptoms and biomarkers for addictive behavior. Some research shows cues, such as the sight and smell of different drugs or alcohol, or contextual clues such as various social situations or environments, trigger and influence drug-seeking behavior.[58] VR can simulate these cues to trigger cravings and consequently help ease them. The preliminary research suggests that VR methods are more effective than traditional exposure therapy methods and help researchers better understand the anxiety, stress, and nervous system responses to the stimuli that trigger addiction.[59]
This research also has implications for not just drug and alcohol addiction but also gambling and food addictions. These insights into how AR/VR can be used to overcome addiction broadly and the use of XR for pain management as a promising alternative or adjunct to opioids could help health researchers better understand opioid addiction and overreliance.[60]
There is a growing body of evidence that VR has the potential to alleviate addiction, which could help address the opioid epidemic in the United States.
Some mental health practitioners believe that engaging patients with psychosis in virtual settings with avatars or voices that resemble their hallucinations may negatively impact patients’ care.[61] However, one study illustrates that VR methods may reduce symptoms and improve physical health, quality of life, and psychosocial functioning in those with psychosis, further illustrating the need to better fund and research the impact of AR/VR on mental health to explore possibilities such as this.[62]
Demographically, both the development of addiction and the onset of psychosis disproportionately affect adolescents and young adults in their early 20s.[63] Because of this population’s high involvement in gaming, “a technological, entertaining, and gaming style intervention may be both relatable to and well-received.”[64] Even for those under 20, a study of 30 children with high-functioning autism shows that VR significantly improved their emotion recognition, attention, and executive function.[65]
Conversely, the elderly also benefit from AR/VR, as it can help connect older adults with family and caregivers, reduce anxiety and stress, and help provide treatment for dementia and other neurological deterioration. According to the World Health Organization (WHO), the number of people ages 60 and older will double by 2050.[66] Research has proven that isolation and loneliness are detrimental for the well-being of the elderly, with the effect of social isolation on mortality comparable to more established risks such as smoking and obesity.[67] AR/VR allows older adults to connect with caregivers in more immersive ways, and one study notes that 9 out of 10 caregivers surveyed said AR/VR technology helped improve their relationships with the elderly they care for.[68]
Use Case: Mynd Immersive’s Elderly Care
Mynd Immersive’s spatial computing software is targeted toward the elderly to provide a variety of therapies, including speech therapy, occupational therapy, anxiety distraction, and the ability to reminisce about past experiences. It is used in senior living communities for long-term care, and also in hospice and palliative care. Through its platform, Mynd Immersive has seen an 88 percent success rate in reducing elders’ feeling of isolation and an 89 percent improvement in socialization.[69]
As more Americans age, loneliness and isolation rates will likely only increase. Loneliness affects up to 60 percent of older Americans and is almost as prevelent as obesity.[70] One Harvard University study finds that loneliness may play a factor in stroke incidence, which is already a leading cause of long-term disability and mortality worldwide.[71] Another Harvard University study states that “being socially isolated carries much greater physical health risks but loneliness has a larger impact on mental-health related conditions.”[72]
By 2054, approximately 23 percent of the U.S. population will be 65 and older.[73] AR/VR provides an opportunity to address this aging population’s rate of feelings of loneliness by creating new ways to engage with family and friends and connect with each other.
Figure 4: Still from Mynd Immersive’s HMD technology in use.[74]

Education
Medical training has been at the forefront of the VR industry; some of the first successful commercial applications of VR were for surgical training simulators in the early 1990s.[75] VR surgical training “allows doctors to practice the mental and physical aspects of complex procedures in a safe, controlled, relaxed environment without risk to real patients.”[76] In addition to the safer environment it creates, VR can also be individualized and customized for different learner needs. Students can learn procedures from some of the top surgeons in the world without having to travel to receive the instruction live. As a result, immersive experiences enhance retention and recall better than 2D learning methods can—90 percent recall for immersive HMDs compared with 78 percent for desktop learning.[77] Indeed, a 2023 HTC Vive survey of 400 surgeons finds that 91 percent believe VR simulation enhances medical education.[78] In addition, research suggests that VR provides the most benefit to education when the training involves technical skills, team training, and decision-making skills—all critical to health care and medical settings.[79]
The medical field has traditionally relied on cadavers (of humans and animals) in order to gain hands-on experience. But this limits the time and number of procedures students can perform on one body, not to mention the logistics and costs of storing and disposing of cadavers, the availability of donors, and the moral and ethical issues associated with using bodies of the deceased. XR provides unlimited opportunities for training of all sorts of procedures without the need for a physical body to perform on. VR training is “portable, relatively inexpensive, and scalable—all features that make it suitable for the medical education setting as a primary or refresher learning tool.”[80] Aside from learning the ins and outs of procedures, XR provides the opportunity for learners to be fully immersed in virtual high-stress or warzone environments, simulating what they would experience on the job rather than in a quiet and sterile cadaveric laboratory.
VR training is “portable, relatively inexpensive, and scalable—all features that make it suitable for the medical education setting as a primary or refresher learning tool.
Medical School and Student Training
Arguably one of the largest use cases for AR/VR in health care today is for medical student training. For medical schools, AR/VR headsets can be a more cost-effective method for student training over the long term than human cadavers or patient simulators.[81] Osso VR found in a study of first-year medical students that those who learned procedures using VR finished 20 percent faster and completed 38 percent more steps correctly than did the traditionally trained students.[82]
In order to make virtual training experiences as realistic as possible, many of these surgical and procedure-based training systems use haptics, which is wearable technology, such as gloves or joysticks, that uses sensors to create tactile experiences alongside the immersive experience. Haptics can simulate the physical resistance of engaging with human tissue, making the training experience more realistic, such as MediViewXR using haptics to simulate needle insertion, mirroring the physical resistance a doctor would encounter on human tissue.[83]
Training is important not to just learn how to do procedures but also how to meet the emotional needs of patients. Simulator-trained residents score significantly higher on assessments of their bedside skills compared with residents who receive traditional training.[84] VR training also allows for simulation of medical emergencies and various scenarios, something students cannot emulate or experience in a lab. For instance, VR can simulate scenarios such as violence in the operating room or an emergency room in the wake of a natural disaster, helping practitioners better prepare for emergencies. This can help students better prepare mentally and physically for various real-world situations they may encounter in their medical careers.
Lastly, some AR/VR programs can provide students with personalized feedback and suggestions for improvement. This is crucial because real-time, tailored feedback allows learners to correct mistakes immediately, reinforcing proper techniques and improving skill retention. Additionally, adaptive learning algorithms can track a student’s progress over time, identifying strengths and weaknesses to customize future training sessions. By providing targeted feedback, AR/VR not only enhances learning efficiency but also ensures that students develop the necessary competencies with greater confidence and precision.[85]
Use Case: Accenture AVENUES Emotional and Empathy Training
Accenture AVENUES is a training tool for public sector workers across child welfare, mental health and addiction services, public assistance, childcare, and health and human services. It immerses users in highly realistic acted scenarios with virtual patients that are designed specifically to evoke responses in users. Its goal is to give users a deeper understanding of their own thought processes when making decisions and developing opinions.[86]
For example, in one module, the user spends time with the patient “Sam” in a telehealth appointment. It is designed to provide an opportunity for health providers to improve their ability to discern pain in telehealth appointments. The goal is to highlight “the role that bias can play in our assumptions about a person’s pain tolerance and believability.”[87]
Another module has users interact with “Jessica,” a Black pregnant mother. The user must make various choices as Jessica is experiencing issues in active labor. The goal of this exercise is for health providers to try out different response scenarios given the pressure of a timely and accurate response in order to save both Jessica and the baby. In the United States, Black women have a maternal mortality rate over twice as high as that of white and Hispanic women.[88] This is another example of illuminating bias in health scenarios, building empathy in practitioners, and balancing emotions in a challenging situation.
In a single lesson, there are 16 quadrillion possible scenarios. The system also gathers user analytics to find behavioral trends and shape future learning agendas.
Empathy and understanding biases are a crucial aspect of medical training. These skills span all kinds of medical professions, from doctors and caregivers to social workers and child care providers. Studies demonstrate that having an empathetic doctor improves patient satisfaction, treatment compliance, and clinical outcomes, in addition to reducing costs for hospitals with lower rates of litigation.[89] Empathy can even lead to more accurate diagnoses, as patients are more likely to divulge more about their symptoms and their concerns.[90]
Figure 5: Accenture AVENUES module, “Jessica”[91]

On-the-Job Training
Because innovations in medicine are constant, doctors and practitioners need refresher courses and training to learn new techniques and treatments, even after graduating from medical school. This is especially important for rural medicine and military combat zones, where providers with limited to no human or animal donor resources can receive effective refresher training before performing a critical procedure.[92] Similar to medical students, they can undergo additional training to address emergency situations in simulated environments.
Doctors widely agree on the need for better training for the trainers themselves. As XR is more widely implemented in medical training, there also needs to be a standard of practice for making sure those that train students and health-care professionals integrate the latest technologies and methods into their curriculums.[93] This wider adoption of XR for training can help eliminate training deserts, or any geographic area where opportunities for continued education in the medical field are difficult to access.[94] However, many hospital administrators recognize the difficulty in committing to train both themselves and their doctors given the time constraints most health-care professionals face today.[95]
Pharmaceutical and Medical Device Researchers and Developers
As medical schools are largely leading the charge for AR/VR use in health care, researchers outside the school system are also using AR/VR to improve the development and trial process of pharmaceutical drugs and medical devices. Emerging technologies such as AI and AR/VR can help provide a better understanding of the underlying biology of diseases and potential treatments by allowing researchers to better model and visualize complex molecular structures, create complex genomic sequences or neural networks, and simulate organ systems or disease progression.[96] Through digital twins, industry can improve medical device design, better identify biomarkers, and speed up biomanufacturing. This could accelerate the drug discovery process, leading to faster development of new treatments and medicines, in addition to saving pharmaceutical researchers time and money.
Emerging technologies such as AI and AR/VR can help provide a better understanding of the underlying biology of diseases and potential treatments by allowing researchers to better model and visualize complex molecular structures, create complex genomic sequences or neural networks, and simulate organ systems or disease progression.
AR/VR applications facilitate better analyses of biological processes that were previously inaccessible through conventional laboratory techniques. Researchers can now immerse themselves in virtual cellular environments, examining molecular interactions at unprecedented resolution and scale. This capability has proved particularly valuable for investigating complex disease mechanisms in conditions such as neurodegenerative disorders and autoimmune diseases, where traditional observational methods often fail to capture the interplay between genetic, environmental, and physiological factors. Furthermore, the collaborative potential of these platforms enables geographically dispersed research teams to simultaneously engage with identical datasets, annotate findings in real time, and collectively evaluate intervention strategies, thereby accelerating the pace of scientific discovery.
The case of Pfizer’s COVID-19 vaccine development illustrates the transformative impact of these technologies on pharmaceutical timelines. It typically takes Pfizer 12 years to develop new medicines. But in 2020, it only took nine months for WHO to approve Pfizer’s COVID-19 vaccine, in part because of Pfizer’s use of digital twins to help upskill workers to improve their retention, efficiency, and speed.[97] Similar approaches could revolutionize the traditionally protracted timeline of therapeutic development and approval.
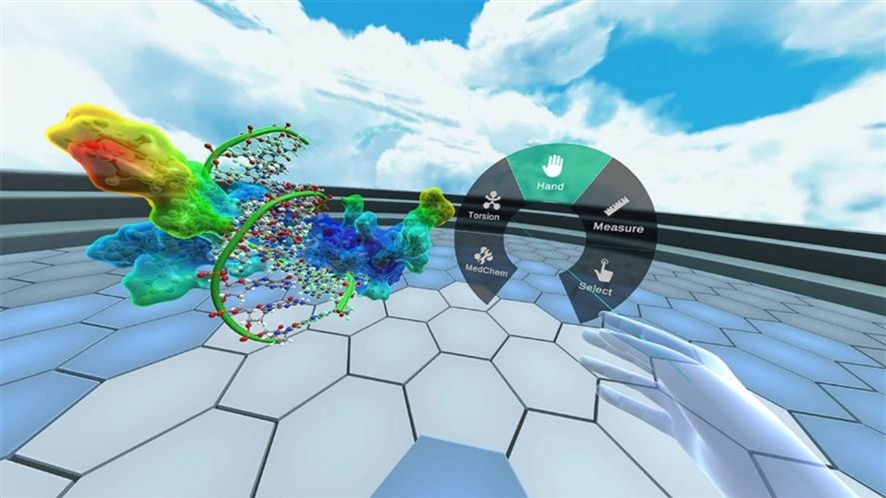
Use Case: Nanome Molecular Modeling
Nanome uses an AI-assisted copilot and multi-user spatial computing for molecular modeling and collaborative drug design. Through VR, researchers can collaborate on drug discovery without having to be in the same location. This technology allows for physical movement within the structures of proteins, helping clinicians better understand both the basis of diseases and the drugs to combat them. For example, researchers at the Oak Ridge National Laboratory, the largest science and energy laboratory in the U.S. Department of Energy, used Nanome to model the 3D architecture of Mpro, which was identified as a target for drug development during the COVID-19 pandemic.[98]
3D molecular modeling can reveal drug designs’ imperfections and prompt revision, preventing costly clinical trial failures. By using AR/VR, Nanome’s application takes 3D modeling a step further by allowing researchers to walk around a structure and manipulate the molecules at a much larger scale. They can also try various simulations and map data onto the structures to test how a molecule will respond. In 2023, Nanome also launched MARA, an AI assistant for molecular analysis and reasoning.[99]
Figure 6: Nanome’s AR application[100]
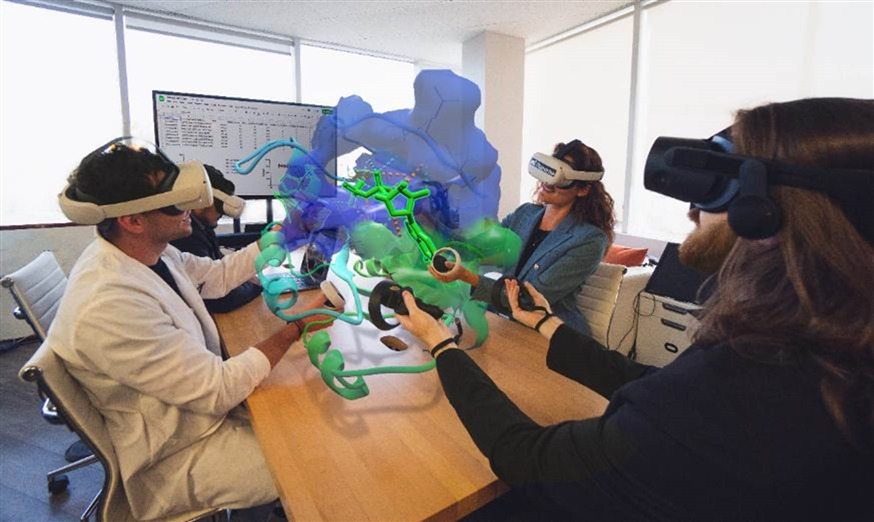
Figure 7: Nanome’s MR application[101]
Patients
The proliferation of wearable health monitoring devices such as smartwatches and rings, alongside connected home fitness equipment including connected bikes and smart mirrors, represents a shift toward technology-mediated personal health empowerment. This transformation, boosted by the COVID-19 pandemic when many consumers invested in home health and fitness equipment during periods of lockdown and social distancing, manifested in unprecedented growth in the home fitness equipment market; sales more than doubled to $2.3 billion between March and October 2020.[102]
AR/VR technologies can facilitate home-based therapeutic interventions that traditionally required clinical settings. This technological advancement addresses critical health-care accessibility challenges across multiple vulnerable populations. For mobility-impaired individuals, AR/VR home treatments eliminate physically demanding and potentially time-exhaustive travel requirements. For rural populations, these technologies mitigate geographic barriers that often result in care postponement or avoidance. Elderly patients particularly benefit, as immersive technologies reduce transportation logistics, minimize exposure to communicable diseases in clinical settings, and enable more consistent care. The confluence of these technologies—wearables, connected fitness equipment, and AR/VR therapeutics—creates a comprehensive health ecosystem that empowers individuals to take charge of their health in a way that saves them hassle, time, and money.
Fitness
Using games for fitness has long predated AR/VR technologies; since 2008, Wii Sports has been the top-selling game for the Wii console, with over 80 million units sold.[103] But headsets provide new ways of engaging in fun fitness activities. According to the Virtual Reality Institute of Health and Exercise, 15 percent of VR games burn enough calories during typical game play to qualify as exercise.[104] Xponential+ is a VR fitness app that has partnered with traditional workout studios such as Pure Barre and Club Pilates to bring their workouts to AR. Instead of traveling to a studio, users can engage with these classes in their own living spaces.[105] AR/VR fitness apps provide personalized fitness classes and training, create fun environments for all skill levels, and ultimately may be cheaper for consumers in the long term.
Just as there are virtual medical assistants, there are also virtual personal trainers. Through a combination of AI and AR/VR, these trainers can provide extremely personalized training in users’ own spaces and at any time. For example, FitXR allows users to take classes at home from professional athletes. In addition, AR/VR fitness has proven to lead to better adherence to exercise. One study finds that aerobic endurance improved in about 76 percent of individuals who participated in video game training compared with traditional methods, and about 53 percent of patients improved in balance, flexibility, and motor coordination.[106]
Just as there are virtual medical assistants, there are also virtual personal trainers. Through a combination of AI and AR/VR, these trainers can provide extremely personalized training in users’ own spaces and at any time.
However, HMDs may be difficult for exercise purposes for some users because of challenges related to user comfort, including the weight, pressure, and tightness of the device on the user’s head and neck. Some frequent VR exercise users find that the band gets too sweaty as they exercise, degrading the quality of the device. As headsets get lighter and users become more comfortable exercising in XR, more consumers will adopt the technology, broadening the scope of people who exercise, while making it easier and more fun.
Use Case: FitXR Fitness
FitXR is a fitness technology company whose FitXR application is one of the most downloaded apps on the Meta Quest store. It has over 1,000 classes available, including combat (e.g., tae kwon do, boxing, karate, and Muay Thai), dance, HIIT (high intensity interval training), pilates, and barre. It also contains games geared toward exercise, such as Slam, which uses AR to combine HIIT with games in one’s home environment. These games can be played with multiple players and users can choose immersive environments to play in such as a gym, seascape, or city rooftop.[107]
Physical activity is important for maintaining good health and fitness, and it contributes to the prevention of noncommunicable diseases such as cardiovascular diseases and diabetes, yet 31 percent of adults do not meet the recommended levels of physical activity. As a result, globally, the cost of physical inactivity on public health systems is about $300 billion.[108]
Figure 8: A FitXR fitness game[109]

Figure 9: A FitXR fitness game[110]

Barriers and Risks to Adoption
Barriers
The integration of AR/VR into the health-care ecosystem faces significant barriers that could impede widespread adoption. These key challenges include integration issues, classification ambiguities, and regulatory burdens. Policymakers and stakeholders will need to work together to address these challenges in order to maximize the benefits of immersive technologies and for the AR/VR industry to reach its full potential in health care.
Integration Challenges
AR/VR headsets have high initial costs for both individual consumers and larger health organizations such as hospitals. However, studies show that long term, AR/VR for training purposes is the more cost-effective option over traditional training programs.[111] Unfortunately, according to the American Hospital Association, in 2022, over half of hospitals closed out the year operating at a loss, while many hospitals spent much of 2023 struggling to break even. Therefore, hospitals are “diverting dollars from their reserves to maintain access to care,” which “has required tradeoffs that have limited many hospitals and health systems from investing in updated infrastructure, new medical technology and equipment, and other clinical needs.”[112] In other words, integrating new technologies such as AR/VR headsets may be financially infeasible for many U.S. hospitals.
These financial burdens are further exacerbated by low staff retention and burnout within the health-care industry; in 2022, 46 percent of health-care workers reported feeling burned out.[113] Resignations per month among health-care workers grew 50 percent between 2020 and 2023.[114] With potentially smaller teams and the need to attract workers with the necessary technological skills and training, integrating AR/VR into these pre-existing clinical workflows may be a challenge. As a result, rural health institutions, those with small, overworked teams, and those with financial constraints may create or exacerbate disparities in treatment, as wealthier communities will be more likely to have access to innovative AR/VR treatments and care.
Health-care systems are actively designing and planning for workforce models that are more sustainable, including by innovating care models, increasing the use of technology, and boosting efforts to attract, recruit, and retain workers. Additionally, education often leads to a more engaged and productive health-care workforce. Workers who feel that their employer is invested in their long-term success are less likely to disengage. Boosting the skills of current employees and training them to perform new roles is more efficient and cost effective than recruiting external talent.[115] Therefore, increasing funding to reskill health-care workers can help build this workforce and increase resiliency.
Unfortunately, the United States’ health-care system is suffering from a lack of retention of highly trained workers, especially in rural areas. The resignation rate per month among health-care workers grew 50 percent between 2020 and 2023.[116] Though the COVID-19 epidemic caused rates of resignation and burnout to spike, a 2024 Mayo Clinic survey finds that 49 percent of physicians experienced burnout, down only 4 percent from the year prior.[117] Nationally, there is also an aging workforce, which is further reflected in the health-care industry. The average age of a registered nurse is 43 years old, and in 2022, less than 17 percent of physicians were under 40 years old.[118]
Lastly, AR/VR can help patients better acclimate to treatment that they may otherwise be unwilling to engage with. As the Veterans Health Administration has stated, VR allows “us to immediately break down barriers of expectation, bias, and resistance to change that hinder [patient] participation.”[119] But there is sometimes a hesitation and lack of comfort with novel technologies because many people still perceive traditional methods as safer and as having more assured outcomes.
Overly Complex Regulations
The health-care industry is heavily regulated in the United States by the FDA, which is charged with “ensuring the safety and efficacy of products and services” related to the medical field, including medical devices.[120] Before any new technology is cleared for use in the American health-care system, the FDA plays a pivotal role in determining its safety and efficacy.[121] What exactly constitutes a medical device, however, is complex. The FDA has approved and given marketing clearance for several applications to be used on AR/VR devices, though some wellness applications do not need FDA approval.[122]
The FDA classifies medical devices based on varying categories of risk, with Class I being the least risky and Class III having the highest level of risk. Class I devices adhere to general controls and include devices such as thermometers and prescription lenses. Class II examples include robotic surgery tools and surgical instruments, while Class III are implantable or life-sustaining devices, which must go through the most rigorous evaluation.[123]
In addition, the 510(k) clearance process is a pathway through which medical device manufacturers seek approval from the FDA. As part of this process, XR technologies can demonstrate substantial equivalence to predicate devices—devices cleared through the 510(k) process and thus legally marketed.[124] Devices that operate similarly to those that have already been approved or cleared by the FDA may not need as intense a review as novel devices do, thereby potentially lowering the requirements for clinical testing of novel devices.[125] Thus, the more AR/VR applications that are approved and given marketing clearance, the more likely further applications will be accepted down the line.
Lastly, the De Novo classification process is a pathway for novel medical devices that do not have a predicate device used as a comparison. This classification typically applies to XR technologies with Class I or Class II risk levels.[126]
Regulating emerging technologies is difficult for the FDA given the pace of innovation and, for AR/VR specifically, the complexities of the technology.[127] Any evaluation methods for new applications or devices should avoid creating unnecessary barriers to the adoption of safe and effective technologies.[128]
Classification Challenges
The FDA has not yet established a specific medical device classification for HMDs. Consequently, the responsibility for gaining regulatory clearance or approval for HMDs in medical contexts has largely fallen on the medical device companies. This presents a significant burden, as HMD manufacturers have not typically submitted their devices to the FDA for marketing as medical devices. Medical device companies that integrate HMDs into their systems often face difficulties in accessing proprietary information vital for FDA submissions, such as material composition for biocompatibility assessments and detailed specifications regarding image quality that meets medical standards. Especially in critical environments such as surgical settings, doctors must be assured that the devices they are using do not have high failure rates, which would include problems such as low latency and low image quality. Medical devices incorporating HMDs must strive to lessen or hopefully remove mental load and cognitive burden on doctors so they can focus on the procedures and patient at hand, instead of the effectiveness and efficiency of the device. Factors such as rendering quality, interactive responsiveness, image quality, latency, and hardware compatibility are all crucial.[129] Low latency while playing a video game is annoying; low latency when performing surgery is life or death.
In addition, usability and ergonomics are crucially important for doctors to make procedures as effective, quick, and error-free as possible.[130] Doctors need a clear field of vision to limit distractions and optimize usability.[131] These usability considerations vary across the spectrum of health-care applications, as VR applications used for immersive therapeutics—such as pain management, exposure therapy for phobias, or rehabilitation exercises—present fundamentally different considerations than do surgical AR applications. The former prioritizes patient comfort and engagement, while the latter demands precision, spatial accuracy, and integration with existing surgical workflows.
Risks
Despite the many benefits and use cases of XR in health care, there are certain risks policymakers should consider. The ultimate goal should be to maximize the benefits of immersive technologies in health care while minimizing the risks through well-crafted, targeted regulations.
Privacy
Many AR/VR applications present unique privacy concerns. These technologies collect large volumes of sensitive personal data, including data from users interacting with virtual environments. Much of the information that AR/VR devices collect is sensitive data not used as often in other consumer technology devices—yet it is critical to the core functions of AR/VR. For example, AR/VR devices may collect eye-gaze and motion-tracking data, which developers need to secure because the information users provide can directly reveal details they may expect would be kept private, such as demographic information, where they live, or how they spend their free time. Concurrently, developers must also ensure that the methods they use to protect user data don’t also decrease the quality of the virtual experiences.[132]
The United States has a multitude of federal and state privacy laws to address specific risks. Many of these laws address data privacy in specific sectors and are not limited to any particular technology. For example, the Privacy Act of 1974 regulates federal agencies’ management of records about individuals, which would include data collected by agencies using AR/VR technologies. Similarly, the Children’s Online Privacy Protection Act (COPPA), the Family Educational Rights and Privacy Act (FERPA), and the Health Insurance Portability and Accountability Act (HIPAA) all regulate data that may be gathered through immersive experiences.
Some of these regulations may leave perceived gaps in privacy protections.[133] For example, COPPA restricts the collection and storage of children’s observed and observable data such as biographical information, audio and video recordings, and geolocation information—but only in products and services intended for children under 13.[134] FERPA applies to schools that receive federal funding and protects students’ education records, giving parents the right to access those records and request the correction of inaccurate information. Schools must also gain students’ (if they are over 18) or their parents’ written consent to disclose their education records.[135] Finally, HIPAA requires patient consent to disclose sensitive health information and gives patients the right to understand that information and control its use.[136] However, HIPAA only applies to certain entities, such as health-care providers, health insurers, intermediaries that facilitate the exchange of health-care data between providers and insurance companies, and those who performs functions such as data analysis or claims processing on behalf of another covered entity.[137]
Though the massive amounts of potentially sensitive data required for using AR/VR within health care requires careful safeguards, addressing user privacy is not unique to immersive technologies and therefore need not be a barrier to innovation or adoption.
Security
Hospitals and health-care institutions are at high risk of cyberattacks, which results in liability concerns, privacy violations, reputational damage, and technical challenges for these institutions.[138] A report by the United Nations finds that more than one-third of responding health institutions reported at least one ransomware attack in 2020.[139] Institutions therefore need to be aware of the security challenges of having connected AR/VR devices within their networks.
A key part of creating secure experiences is usability. For AR/VR technologies, one aspect of usability is authenticating users, or the process of confirming a user is who they claim to be, typically performed via credentials such as passwords, security questions, mobile devices, ID cards, or biometric data such as fingerprints, voiceprints, or facial features. The goal of authentication is to ensure that only authorized users can access sensitive information or restricted services. To ensure that only authorized doctors and nurses can access HMDs, especially because of the highly sensitive and individual personal information at risk, health-care institutions should prioritize usable security features. One challenge with the shift to AR/VR technology is that the methods that work well for authenticating users in 2D digital spaces are more difficult to use with immersive technologies, meaning the security challenges associated with AR/VR are even more complex than those associated with other technologies.[140]
The ultimate goal should be to maximize the benefits of immersive technologies in health care while minimizing the risks through well-crafted, targeted regulations.
Adverse Health Impacts
Using AR/VR devices for extended periods of time may have adverse health impacts on users. For example, cybersickness is the body’s response to the incongruity between the visual information from a VR headset and the body’s sense of movement or position after prolonged use of a headset. Cybersickness symptoms include unstable posture, shifts in vision, and altered hand-eye coordination.[141]
As is the case with prolonged computer monitor, television screen, or smartphone use, eye strain is a common issue when using an AR/VR device for extended periods of time. Headsets can potentially affect users’ ability to focus, track objects, and perceive depth. However, more research and data are needed to make definitive conclusions, especially because most findings so far have found negligible and only minor long-term impacts. As it pertains to patients themselves using devices, research should particularly focus on children, whose visual systems are still developing, and individuals who may be more susceptible to already weak eye movement or control, such as those with cerebral palsy or Down syndrome.[142]
Lastly, there are concerns over addiction to immersive experiences, similar to concerns expressed over social media addiction, particularly for youth. While there is still a need for further research regarding any addictive nature of AR/VR devices, technology companies should continue to adopt user and parental controls such as screen-time limits and prompts to take breaks after using a device for an extended period of time.[143]
Policy Recommendations
Given the abundant use cases for XR in health care, policymakers should incentivize the industry to innovate and develop and avoid overly restrictive legislation while still addressing the potential risks. Such an approach should include supporting privacy-enhancing data-sharing practices, promoting AI in health applications, funding medical education and workforce development, improving the FDA approval pipeline, ensuring that AR/VR technologies are included in Medicare and Medicaid coverage, developing standards, and funding research into AR/VR’s impact on public health.
Support Federal Privacy Legislation to Create Consistent Protection of AR/VR Data
Congress should pass comprehensive data privacy legislation that streamlines regulation, preempts state laws, establishes basic consumer data rights, and minimizes the impact on innovation. Such legislation would ensure that both regulators and developers consistently implement necessary privacy safeguards as AR/VR technologies continue to evolve.
Regulators should ensure that requirements are consistent across sector-specific regulations, and any such specific requirements augment, rather than contradict or complicate, broader federal privacy legislation. Such an approach could address potentially conflicting compliance requirements and set clear standards for user privacy protections for both existing and emerging data collection practices in AR/VR.
For instance, the Department of Health and Human Services (HHS) may consider which observable, observed, and resulting computed data gathered by AR/VR constitutes “protected health information” under HIPAA when these technologies are used in health care. As more health-care institutions share data and patient information to better adopt AR/VR in their treatments, HHS should clarify these guidelines for HIPPAA.[144]
Promote Public-Private Partnerships to Advance AR/VR Health-Care Innovation
Public-private partnerships play an important role in advancing AR/VR technologies in health care because these collaborations merge governmental resources, regulatory expertise, and public health priorities with private sector technological capabilities and market knowledge. These complementary strengths address several of the barriers to AR/VR implementation such as regulatory complexity and implementation challenges. Furthermore, such partnerships create innovation ecosystems wherein risk sharing enables more ambitious technological development and establishes channels for knowledge transfer between the sectors.
For example, NIH’s BRAIN (Brain Research Through Advancing Innovative Neurotechnologies) Initiative is a public-private partnership that aims to accelerate the development of neurotechnologies, including AR/VR.[145] This partnership is funded through Congress—which itself should ensure collaborations such as this are continually funded, as this funding has decreased since 2024 and is set to end in 2026.[146]
There are also many academic consortia studying and developing XR applications in health care, which are helping inform clinical practice and standards. For example, the Center for Medical Innovation in Extended Reality (MIXR) is a National Science Foundation (NSF)-supported group working within academia, industry, and government to explore XR applications in public health, medical education, and clinical care.[147] NSF should continue to fund research on the impact of XR in health care and grow the evidence base for the benefits of using this technology over traditional care methods.
Furthermore, the development of AI applications applicable to AR/VR, such as natural language processing and machine learning (ML), will spur further innovation in AR/VR. Government funding of AI supports foundational research, such as AI studies on new drug development algorithms and basic science applications of AI that may not yield immediate commercial returns but can pave the way to major breakthroughs and further incentivize private sector investment. By funding research without direct commercial application or with high uncertainty, public funding can foster innovation that might otherwise be missed. Moreover, public funding can help increase efficiencies, de-risk early stage innovation, and ensure that AI tools address public health needs, enhancing health equity.[148]
Public funding also encourages open science and collaboration, resulting in the creation of public goods such as large datasets, tools, and infrastructure that are available to all agents in the health ecosystem. Finally, public funding can address ethical and privacy concerns by ensuring that AI development aligns with guidelines such as fairness, transparency, and the mitigation of bias to support equitable AI-enabled development.[149]
Increased Integration of AR/VR in Health-Care Education and Workforce Development Programs
In order to address the aging health-care workforce, decrease burnout, and ensure retention through highly skilled training, federal agencies should encourage better integration of AR/VR for federally supported health workforce education programs. HHS and the Health Resources and Services Administration have existing health workforce programs aimed at improving the health-care workforce and care deserts, but neither explicitly include ways to integrate AR/VR training into them.[150] In addition, the Department of Labor’s Employment and Training Administration should better expand its existing programs to include AR/VR health-care training.[151] Federal agencies are well placed to implement these programs and fund others through their subsequent grant programs as well.[152]
Improve FDA Approval Process for AR/VR Technologies
Though the FDA determines the safety and efficacy of medical technologies before health-care providers can use them in clinical settings, the FDA itself has said that it “recognize[s] there is a need to enhance and adapt the 510(k) Program to best advance more modern technologies.”[153] To ensure that the FDA continues to approve AR/VR applications, the agency should better incentivize more companies to use its Breakthrough Devices Program (BDP), which is designed to expedite the review of medical devices that provide more effective treatment or diagnosis for life-threatening diseases and improve communication with FDA officials.
This designation helps prevent delays in the FDA’s review of devices by providing manufacturers with access to FDA experts to address topics as they arise during the premarket review phase.[154] For technologies that “significantly improve the safety of currently available treatments or diagnostics” that treat less-serious issues than those covered by the BDP, the FDA also has a similar program called the Safer Technologies Program (STeP). The goal of both of these programs is to provide patients and physicians with access to innovative medical devices by expediting their development, assessment, and review process.[155] As research points to the effectiveness of AR/VR devices, the FDA should continue to recognize the importance of encouraging the growth of innovative technologies by ensuring that it is staffed with experts capable of understanding the technical aspects needed for an expedient approval process.[156]
Even though devices given a STeP or BDP designation are treated as a priority by the FDA, the regulatory burden is not reduced; it does not negate the testing and trial processes nor replace the 510(k) process. Fortunately, in 2024, the FDA designated more products under the BDP than it did in 2023.[157]
In addition, the FDA should continue to work with and fund the National Evaluation System for health Technology (NEST) at the Medical Device Innovation Consortium, which coalesces and generates research into the effectiveness of innovative technologies in health care. NEST researches ways to improve regulatory pipelines and evaluate medical devices more effectively.[158]
Ensure That AR/VR Technologies Are Included in Medicare and Medicaid Coverage
For U.S. health-care insurers, the Healthcare Common Procedure Coding System (HCPCS) provides a standardized classification system so Medicare and other health insurance programs can process claims consistently. The American Medical Association (AMA) maintains the coding system that primarily identifies medical services and procedures performed by physicians or other health-care professionals as comprising procedures found in the Current Procedural Terminology (CPT). In 2022, the AMA approved the first ever CPT code for VR therapy.[159]
The Centers for Medicare and Medicaid Services (CMS) is also already valuing the efficacy of AR/VR therapeutics. RelieVRx, a VR experience for helping with chronic lower back pain, is the first “immersive therapeutic to be included in an existing benefit category.”[160] CMS gave AppliedVR, RelieVRx’s parent company, an HCPCS Level II code as durable medical equipment.[161]
Typically, however, Medicare coverage only pays for items and services that are “reasonable and necessary” to treat an illness or injury, thereby mostly excluding experimental services or products. As a result, it usually takes an average of five years for an FDA-approved product or device to receive Medicare coverage.[162] In response, CMS created the Coverage with Evidence Development (CED) program in 2005, which gives Medicare beneficiaries access to new medical technologies.[163] Unfortunately, CED has only approved a handful of technologies, and has not updated the data collection process despite recent advances in data collection and analysis.[164]
In his first term, President Trump’s administration created the Medicare Coverage of Innovative Technologies (MCIT) rule, which would have designated same-day Medicare coverage to any product or service granted BDP approval.[165] The Biden administration repealed MCIT, so to modify CED and build off MCIT, in August 2024, CMS announced the Transitional Coverage of Emerging Technologies (TCET), which aims to expedite Medicare coverage of BDP devices by encouraging Medicare benefit category determination, coding, and payment reviews of new technologies, “further helping translate innovation into meaningful patient access.”[166] TCET also seeks to improve the Medicare coverage review process between CMS and industry.
While TCET will hopefully shorten the timelines for Medicare decision-making and improve communication between CMS officials and industry, CMS limits TCET to only five devices a year.[167] There are also still issues with CMS’s data collection processes, according to medical researchers at Tufts Medical Center: “Data collection through CED-approved clinical trials and registries has often proven costly and prolonged, and yielded evidence of variable quality and relevance.”[168]
Congress has previously tried and failed to codify MCIT into law, with bills such as the Ensuring Patient Access to Critical Breakthrough Products Act of 2024.[169] CMS should continue to label and approve AR/VR treatments in order to ensure that Medicare and Medicaid cover AR/VR treatments. It is important to note that the FDA must first approve an application before CMS can approve it. Second, Congress should clarify CMS’s “reasonable and necessary” language to better include immersive and emerging technologies and broaden TCET’s remit to include more technologies, widen the scope of data it collects, and study new treatments with emerging technologies. Furthermore, CMS’s approval of immersive technologies should help entice and make private insurers aware of the benefits of these applications, as CMS approval typically signals to private insurance to cover the technology too. Lastly, Congress should ensure that Medicare and Medicaid coverage includes funding for telehealth services.[170]
Continue to Develop Standards for AR/VR In Health Care
The medical industry needs better standards and evaluation methods for medical image quality in AR/VR devices. Because doctors require high-quality images and use commercially available software and game engines for their rendering, standards should better incorporate the necessity of high-quality images for medical purposes. The International Electrotechnical Commission (IEC) has developed image quality standards for near-eye displays, while the International Organization for Standardization (ISO) has developed similar standards, mostly regarding ergonomics.[171] Generally, the health-care industry uses the Digital Imaging and Communications in Medicine (DICOM) Grayscale Standard Display Function for image quality as well. In addition, the American Association of Physicists in Medicine has developed procedures for medical displays. Despite all these standards’ implications for HMDs and XR applications, they thus far have not described the processing of medical images and DICOM data to create 3D virtual objects. Developers often use off-the-shelf hardware for MXR applications without having full control over that hardware, making standards development particularly important to standardize image quality and ergonomics.[172]
There are several groups that are well placed to promulgate developments and drive industry standards in medical applications of MXR. The International Virtual Reality and Healthcare Association’s founding members include 8 universities, 5 research institutions, and 27 technology companies. This consortium aims to coordinate and develop industry standards around AR/VR for medical systems.[173] Similarly, the American Medical Extended Reality Association consists of 300 members including physicians, nurses, researchers, and universities whose members include Cedars Sinai, the Massachusetts Institute of Technology, Mass General Brigham, and NIH.
Continue to Fund Research Into Immersive Technologies’ Impact on Public Health
The U.S. Veterans Health Administration (VHA), a leader in the XR and rehabilitation space, has more than 75 sites using XR today.[174] They utilize AR/VR experiences to treat veterans for pain management, physical rehabilitation, and mental health care. Congress should continue to allocate funds to the VHA for its work in utilizing and experimenting with XR. In late April 2025, the Congressional Virtual, Augmented, and Mixed Reality Caucus submitted requests to the House Appropriations Committee to continue prioritizing AR/VR’s importance for veterans’ mental health, among other priorities.[175]
The Artificial Intelligence and Machine Learning Program in the FDA’s Center for Devices and Radiological Health (CDRH) conducts regulatory science research to ensure patient access to safe and effective medical devices using AI/ML.[176] This group should also look into AR/VR devices as part of this work stream.
Any research setting should include feedback from end users, particularly those with disabilities. Research should ensure that the technology is fully accessible to accommodate for a plethora of health disparities.[177]
Conclusion
From aiding with patients’ overreliance on opioids to revolutionizing surgery, XR is revolutionizing the health-care industry that is empowering patients to take control of their health in novel ways. This technology will improve access to the best possible levels of care for all patients, especially those in underserved communities and rural areas. It also emboldens health-care workers to learn the most cutting-edge techniques, both ensuring that the American workforce is well trained and competitive and increasing workers’ likelihood to stay in the medical field. As the health-care industry innovates and AR/VR technologies improve, the integration of these technologies into the health-care system will ensure American competitiveness in medical innovation while simultaneously improving patient outcomes and experiences.
Acknowledgments
The author would like to thank Daniel Castro, Ash Johnson, Sandra Barbosu, Stephen Ezell, Adam Cargill, and Peirce Clark for their feedback and input on this report. Any errors or omissions are the author’s own.
About the Author
Alex Ambrose is a policy analyst at ITIF focusing on augmented and virtual reality, as well as children’s online safety and privacy. She previously worked at ITIF as a communications manager. She holds a B.S. in public relations from Syracuse University and an M.P.A. in public policy analysis from Indiana University.
About ITIF
The Information Technology and Innovation Foundation (ITIF) is an independent 501(c)(3) nonprofit, nonpartisan research and educational institute that has been recognized repeatedly as the world’s leading think tank for science and technology policy. Its mission is to formulate, evaluate, and promote policy solutions that accelerate innovation and boost productivity to spur growth, opportunity, and progress. For more information, visit itif.org/about.
Endnotes
[1]. “Augmented Reality and Virtual Reality Medical Devices: Questions to Consider,” Food and Drug Administration, accessed on December 12, 2024, https://www.fda.gov/medical-devices/digital-health-center-excellence/augmented-reality-and-virtual-reality-medical-devices-questions-consider.
[2]. “XR Association Developer’s Guide: Chapter 5, Designing Immersive Solutions for Healthcare,” XR Association, December 2023.
[3]. Louis Rosenberg, “Augmented Reality: Reflections at Thirty Years,” Future Technologies Conference, October 2021, https://www.researchgate.net/publication/353753442_Augmented_Reality_Reflections_at_Thirty_Years.
[4]. Alvin W. Graylin and Louis Rosenberg, Our Next Reality: How the AI-powered Metaverse Will Reshape the World (Boston: Nicholas Brealey, 2024), 207–242.
[5]. “Virtual Reality (VR) in Healthcare Market Size, Share & Industry Analysis, By Component (Hardware, Software, and Content), By Application (Pain Management, Education & Training, Surgery, Patient Care Management, Rehabilitation & Therapy Procedures, and Others), and Regional Forecast, 2024-2032,” Fortune Business Insights, December 23, 2024, https://www.fortunebusinessinsights.com/industry-reports/virtual-reality-vr-in-healthcare-market-101679.
[6]. “Insights on the Future of XR in Healthcare,” XR Association, accessed on December 16, 2024, https://xra.org/research/insights-on-the-future-of-xr-in-healthcare/.
[7]. Ellysse Dick, “The Promise of Immersive Learning: Augmented and Virtual Reality’s Potential in Education” (ITIF, August 30, 2021), https://itif.org/publications/2021/08/30/promise-immersive-learning-augmented-and-virtual-reality-potential/.
[8]. Juan Londoño, “User Safety in AR/VR: Protecting Adults” (ITIF, January 17, 2023) https://itif.org/publications/2023/01/17/user-safety-in-ar-vr-protecting-adults/.
[9]. Andrea Volpe, “The Question of Care,” Harvard Medicine, 2019, https://magazine.hms.harvard.edu/articles/question-care.
[10]. Jyoti Kumari et al., “Metaverse in diagnosis of skin diseases,” Journal of Cosmetic Dermatology, Vol. 22, Issue 2 (2022), https://onlinelibrary.wiley.com/doi/10.1111/jocd.15409; Christian Jung et al., “Virtual and Augmented Reality in Cardiovascular Care,” American College of Cardiology Foundation, Vol. 15, No. 3 (2022), https://www.jacc.org/doi/epdf/10.1016/j.jcmg.2021.08.017; Weronika Magdalena Zydowicz et al., “Current Trends and Beyond Conventional Approaches: Advancements in Breast Cancer Surgery through Three-Dimensional Imaging, Virtual Reality, Augmented Reality, and the Emerging Metaverse,” Journal of Clinical Medicine, Vol. 13 (2024), https://doi.org/10.3390/jcm13030915.
[11]. Graylin and Rosenburg, Our Next Reality: How the AI-powered Metaverse Will Reshape the World.
[12]. Juan Londoño, “The United States Is Already Playing Catch Up With Digital Twins” (ITIF, November 9, 2023), https://itif.org/publications/2023/11/09/united-states-is-already-playing-catch-up-with-digital-twins/.
[13]. “XR Association Developer’s Guide: Chapter 5, Designing Immersive Solutions for Healthcare,” XR Association, December 2023.
[14]. Alexandre Vallée, “Digital twin for healthcare systems,” Frontiers in Digital Health, September 2023, https://pmc.ncbi.nlm.nih.gov/articles/PMC10513171/.
[15]. Ryan Beams et al., “Evaluation Challenges for the Application of Extended Reality Devices in Medicine,” Journal of Digital Imaging (November 2021), https://link.springer.com/article/10.1007/s10278-022-00622-x.
[16]. Ibid.
[17]. Center for Medical Innovations in Extended Reality conference discussion, Washington DC, October 3, 2024.
[18]. Brent Felix et al., “Augmented Reality Spine Surgery Navigation: Increasing Pedicle Screw Insertion Accuracy for Both Open and Minimally Invasive Spine Surgeries,” Spine, June 15, 2022, https://pubmed.ncbi.nlm.nih.gov/35132049/; Graylin and Rosenburg, Our Next Reality: How the AI-powered Metaverse Will Reshape the World.; Ahmed A. Aoude et al., “Methods to determine pedicle screw placement accuracy in spine surgery: A systematic review,” Eur Spine J. 2015, https://pubmed.ncbi.nlm.nih.gov/25749690.
[19]. Graylin and Rosenburg, Our Next Reality: How the AI-powered Metaverse Will Reshape the World.
[20]. “XR Association Developer’s Guide: Chapter 5, Designing Immersive Solutions for Healthcare,” XR Association, December 2023.
[21]. “Technology,” MediView, accessed on April 12, 2025, https://mediview.com/technology/.
[22]. “Mediview XR90,” MediView, retrieved on November 14, 2024, https://mediview.com/mediview-xr90-2/; “In Focus: Holographic Heads up Display,” MediView, accessed on November 14, 2024, https://www.youtube.com/watch?v=vKYKgDJxJCA.
[23]. “Augmented Reality and Virtual Reality in Medical Devices: 7 Questions to Consider When Talking to Your Health Care Professional About Using Augmented Reality and Virtual Reality in Your Care,” Food and Drug Administration, accessed on December 12, 2024, https://www.fda.gov/media/176814/download.
[24]. Luana Colloca et al., “Virtual reality: physiological and behavioral mechanisms to increase individual pain tolerance limits,” Pain, 2020, https://pubmed.ncbi.nlm.nih.gov/32345915/.
[25]. Graylin and Rosenburg, Our Next Reality: How the AI-powered Metaverse Will Reshape the World.
[26]. Hunter G. Hoffman et al., “Virtual reality hand therapy: A new tool for nonopioid analgesia for acute procedural pain, hand rehabilitation, and VR embodiment therapy for phantom limb pain,” Journal of Hand Therapy, Vol. 33, Issue 2, (April-June 2020), 254–262, https://www.jhandtherapy.org/article/S0894-1130(20)30078-8/abstract.
[27]. Hunter G. Hoffman et al., “Virtual Reality Pain Control During Burn Wound Debridement in the Hydrotank,” The Clinical Journal of Pain, Vol. 24 (May 2008), https://journals.lww.com/clinicalpain/abstract/2008/05000/virtual_reality_pain_control_during_burn_wound.4.aspx; Zydowicz et al., “Current Trends and Beyond Conventional Approaches: Advancements in Breast Cancer Surgery through Three-Dimensional Imaging, Virtual Reality, Augmented Reality, and the Emerging Metaverse.”
[28]. Helen Ouyang, “Can Virtual Reality Help Ease Chronic Pain?” The New York Times, June 15, 2023, https://www.nytimes.com/2022/04/26/magazine/virtual-reality-chronic-pain.html; “Cedars-Sinai Medical Center Overview,” U.S. News and World Report, accessed on January 10, 2025, https://health.usnews.com/best-hospitals/area/ca/cedars-sinai-medical-center-6930444.
[29]. “Our Research and Clinical Trials,” Applied VR, accessed on January 10, 2025, https://www.appliedvr.io/research.
[30]. Ibid.
[31]. “Diaphragmatic Breathing,” Johns Hopkins Medicine, accessed on April 14, 2025, https://www.hopkinsmedicine.org/all-childrens-hospital/services/anesthesiology/pain-management/complimentary-pain-therapies/diaphragmatic-breathing.
[32]. “Newsroom,” Applied VR, accessed on January 10, 2025, https://www.appliedvr.io/news.
[33]. “Therapy,” Smileyscope, accessed on January 10, 2025, https://www.smileyscope.com/; “Smileyscope Therapy is the First Virtual Reality Device to Receive FDA Class II Clearance for Acute Pain,” Smileyscope, November 6, 2023, https://www.prweb.com/releases/smileyscope-therapy-is-the-first-virtual-reality-device-to-receive-fda-class-ii-clearance-for-acute-pain-301978129.html.
[34]. Alex Ambrose, “User Safety in AR/VR: Protecting Kids” (ITIF, September 3, 2024), https://itif.org/publications/2024/09/03/user-safety-in-ar-vr-protecting-kids/.
[35]. “Augmented Reality and Virtual Reality in Medical Devices: 7 Questions to Consider When Talking to Your Health Care Professional About Using Augmented Reality and Virtual Reality in Your Care,” Food and Drug Administration; Ambrose, “User Safety in AR/VR: Protecting Kids.”
[36]. “Toolbox,” Smileyscope, accessed on January 10, 2025, https://www.smileyscope.com/professionals.
[37]. Onyi Lam, Brian Broderick, and Skye Toor, “How far Americans live from the closest hospital differs by community type,” Pew Research Center, December 12, 2018, https://www.pewresearch.org/short-reads/2018/12/12/how-far-americans-live-from-the-closest-hospital-differs-by-community-type/.
[38]. “More than half of the global rural population excluded from health care,” International Labor Organization, April 27, 2015, https://www.ilo.org/resource/news/more-half-global-rural-population-excluded-health-care.
[39]. Graylin and Rosenburg, Our Next Reality: How the AI-powered Metaverse Will Reshape the World.
[40]. Sandee LaMotte, “The very real health dangers of virtual reality,” CNN, December 13, 2017, https://www.cnn.com/2017/12/13/health/virtual-reality-vr-dangers-safety/index.html.
[41]. “Virtual Reality,” American Physical Therapy Association, accessed on January 2, 2025, https://www.apta.org/patient-care/interventions/virtual-reality.
[42]. Ryan Beams et al., “Evaluation Challenges for the Application of Extended Reality Devices in Medicine,” Journal of Digital Imaging (November 2021), https://link.springer.com/article/10.1007/s10278-022-00622-x; “Neuro Rehab VR: Interdisciplinary Neurorehabilitation (Physical, Occupational and Recreational) Therapy and Spinal Cord Injury and Disorder (SCI/D),” U.S. Department of Veterans Affairs, retrieved on December 23, 2024, https://marketplace.va.gov/innovations/neuro-rehab-vr.
[43]. “VIVE Ultimate Tracker,” VIVE, accessed on April 15, 2025, https://www.vive.com/us/accessory/vive-ultimate-tracker/.
[44]. “Virtualis PhysioVR,” e3 Diagnostics, accessed on April 17, 2025, http://e3diagnostics.com/products/vestibular---balance/virtualis-physiovr.
[45]. “Online Physical Therapy,” XR Health, accessed on April 17, 2025, https://www.xr.health/us/services/physical-rehabilitation/.
[46]. Anne Bailey, “VA expands virtual reality for Veteran rehabilitation,” U.S. Department of Veterans Affairs, April 3, 2023, https://news.va.gov/117227/va-expands-virtual-reality-rehabilitation/.
[47]. C. Pazzaglia et al., “Comparison of virtual reality rehabilitation and conventional rehabilitation in Parkinson’s disease: a randomized controlled trial,” Physiotherapy, Vol. 106 (2020), 36-42, https://www.sciencedirect.com/science/article/abs/pii/S0031940618301287.
[48]. “Virtual reality technology and individuals with communication disorders,” Illinois State University, October 13, 2023, https://news.illinoisstate.edu/2023/10/virtual-reality-technology-and-individuals-with-communication-disorders/; Sophie Brassel et al., “Speech-Language Pathologists’ Views of Using Virtual Reality for Managing Cognitive-Communication Disorders Following Traumatic Brain Injury,” American Speech-Language-Hearing Association, September 8, 2022, https://pubmed.ncbi.nlm.nih.gov/36580534/.
[49]. Brassel et al., “Speech-Language Pathologists’ Views of Using Virtual Reality for Managing Cognitive-Communication Disorders Following Traumatic Brain Injury.”
[50]. Lucy Lan et al., “A Systematic Review of using Virtual and Augmented Reality for the Diagnosis and Treatment of Psychotic Disorders,” Curr Treat Options Psych, Vol. 10 (2023), 87–107, https://doi.org/10.1007/s40501-023-00287-5.
[51]. Ibid.
[52]. “Information about Mental Illness and the Brain,” National Institutes of Health, 2007, https://www.ncbi.nlm.nih.gov/books/NBK20369/.
[53]. Getinet Ayano et al., “Misdiagnosis, detection rate, and associated factors of severe psychiatric disorders in specialized psychiatry centers in Ethiopia,” Annals of General Psychiatry, Vol. 20 (2021), https://annals-general-psychiatry.biomedcentral.com/articles/10.1186/s12991-021-00333-7.
[54]. Monica Vermani, Madalyn Marcus, and Martin A. Katzman, “Rates of Detection of Mood and Anxiety Disorders in Primary Care: A Descriptive, Cross-Sectional Study,” The Primary Care Companion for CNS Disorders, 2011, https://pmc.ncbi.nlm.nih.gov/articles/PMC3184591/.
[55]. Shelby Bradford, “How Augmented Reality is Advancing Brain and Mental Health Treatment,” The Scientist, March 7, 2025, https://www.the-scientist.com/how-augmented-reality-is-advancing-brain-and-mental-health-treatment-72757.
[56]. Lan et al., “A Systematic Review of using Virtual and Augmented Reality for the Diagnosis and Treatment of Psychotic Disorders.”
[57]. Ibid.
[58]. Massimiliano Mazza et al., “Virtual reality: a powerful technology to provide novel insight into treatment mechanisms of addiction,” Translational Psychiatry, 2021, https://www.nature.com/articles/s41398-021-01739-3.
[59]. Ibid.
[60]. “Augmented Reality and Virtual Reality Medical Devices: Questions to Consider,” Food and Drug Administration, accessed on December 12, 2024, https://www.fda.gov/medical-devices/digital-health-center-excellence/augmented-reality-and-virtual-reality-medical-devices-questions-consider
[61]. Lan et al., “A Systematic Review of using Virtual and Augmented Reality for the Diagnosis and Treatment of Psychotic Disorders.”
[62]. Ibid.
[63]. Lan et al., “A Systematic Review of using Virtual and Augmented Reality for the Diagnosis and Treatment of Psychotic Disorders”; Nathan Yerby, “Addiction Statistics,” Addiction Center, accessed on April 12, 2025, https://www.addictioncenter.com/addiction/addiction-statistics/.
[64]. Lan et al., “A Systematic Review of using Virtual and Augmented Reality for the Diagnosis and Treatment of Psychotic Disorders”; Ambrose, “User Safety in AR/VR: Protecting Kids.”
[65]. Lan et al., “A Systematic Review of using Virtual and Augmented Reality for the Diagnosis and Treatment of Psychotic Disorders.”
[66]. Lee Woodruff, “The Promise of AR/VR and Neuro Stimulation in Family Caregiving,” AARP, September 30, 2024, https://www.aarp.org/caregiving/basics/info-2024/ar-vr-for-caregivers.html.
[67]. “Social Isolation and Loneliness,” World Health Organization, retrieved on January 8, 2024, https://www.who.int/teams/social-determinants-of-health/demographic-change-and-healthy-ageing/social-isolation-and-loneliness.
[68]. Woodruff, “The Promise of AR/VR and Neuro Stimulation in Family Caregiving.”
[69]. Mynd Immersive, “Who We Are,” retrieved on March 5, 2025, https://www.myndimmersive.com/vr-based-digital-therapeutics.
[70]. “The power and prevalence of loneliness,” Harvard Health Publishing, January 13, 2017, https://www.health.harvard.edu/blog/the-power-and-prevalence-of-loneliness-2017011310977.
[71]. “Chronic loneliness may increase stroke risk among older adults,” Harvard University, June 24, 2024, https://hsph.harvard.edu/news/chronic-loneliness-may-increase-stroke-risk-among-older-adults/.
[72]. Alvin Powell, “How social isolation, loneliness can shorten life,” The Harvard Gazette, October 3, 2023, https://news.harvard.edu/gazette/story/2023/10/how-social-isolation-loneliness-can-shorten-your-life/.
[73]. Katherine Schaeffer, “U.S. centenarian population is projected to quadruple over the next 30 years,” Pew Research Center, January 9, 2024, https://www.pewresearch.org/short-reads/2024/01/09/us-centenarian-population-is-projected-to-quadruple-over-the-next-30-years/.
[74]. “Senior Living,” Mynd Immersive, accessed on April 14. 2025, https://www.myndimmersive.com/senior-living.
[75]. Graylin and Rosenburg, Our Next Reality: How the AI-powered Metaverse Will Reshape the World.
[76]. Ibid.
[77]. Eric Krokos, Catherine Plaisant, Amitabh Varshney, “Virtual memory palaces: immersion aids recall,” Virtual Reality, (2019), https://obj.umiacs.umd.edu/virtual_reality_study/10.1007-s10055-018-0346-3.pdf.
[78]. “Survey Results: The State of Extended Reality Training in Healthcare,” HTC Vive, 2023, https://business.vive.com/us/stories/vr-healthcare-survey-report-2023/.
[79]. Heather Groves et al., “Assessing the Efficacy of Virtual Reality Trauma Surgery Training as Compared to Cadaveric Training,” DOI, August 1, 2023, https://doi.org/10.21203/rs.3.rs-3147922/v1.
[80]. Ibid.
[81]. Alivia Kaylor, “How Virtual Reality Could Reform Surgical Training,” TechTarget, December 19, 2022, https://www.techtarget.com/pharmalifesciences/answer/How-Virtual-Reality-Could-Reform-Surgical-Training.
[82]. “New Study Shows Virtual Reality Training Outperforms Traditional Methods in Orthopedic Surgical Education,” Osso VR, November 9, 2023, https://www.ossovr.com/press-releases/vr-training-outperforms-traditional-methods-in-orthopedic-surgical-education.
[83]. “Mediview XR90,” MediView, retrieved on October 29, 2024, https://mediview.com/mediview-xr90-2/; Graylin and Rosenburg, Our Next Reality: How the AI-powered Metaverse Will Reshape the World.
[84]. Groves et al., “Assessing the Efficacy of Virtual Reality Trauma Surgery Training as Compared to Cadaveric Training.”
[85]. “New Study Shows Virtual Reality Training Outperforms Traditional Methods in Orthopedic Surgical Education,” Osso VR.
[86]. Accenture AVENUES, accessed on January 7, 2025, https://www.accenture.com/us-en/services/public-service/caseworker-virtual-reality.
[87]. Ibid.
[88]. Donna L Hoyert, “Maternal Mortality Rates in the United States, 2021,” National Center for Health Statistics, 2021, https://www.cdc.gov/nchs/data/hestat/maternal-mortality/2021/maternal-mortality-rates-2021.htm.
[89]. Ted A. James, “Building Empathy into the Structure of Health Care,” Harvard Medical School, January 12, 2023, https://postgraduateeducation.hms.harvard.edu/trends-medicine/building-empathy-structure-health-care.
[90]. Gemma McNally et al., “Teaching empathy to medical students,” Association for the Study of Medical Education, December 22, 2022, https://asmepublications.onlinelibrary.wiley.com/doi/10.1111/tct.13557.
[91]. “AVENUES,” Accenture, accessed on January 10, 2025, https://www.accenture.com/us-en/services/public-service/caseworker-virtual-reality.
[92]. Groves et al., “Assessing the Efficacy of Virtual Reality Trauma Surgery Training as Compared to Cadaveric Training.”
[93]. Center for Medical Innovations in Extended Reality conference discussion, Washington DC, October 3, 2024.
[94]. Ibid.
[95]. “3 Challenges of Technology Implementation in Healthcare,” University of Southern California, November 17, 2023, https://healthadministrationdegree.usc.edu/blog/3-challenges-of-technology-implementation-in-healthcare.
[96]. Sandra Barbosu, “Harnessing AI to Accelerate Innovation in the Biopharmaceutical Industry” (ITIF, November 15, 2024), https://itif.org/publications/2024/11/15/harnessing-ai-to-accelerate-innovation-in-the-biopharmaceutical-industry/; “How Virtual Reality Takes Scientists Inside New Molecules,” Pfizer, retrieved on January 7, 2025, https://www.pfizer.com/news/articles/how_virtual_reality_takes_scientists_inside_new_molecules_video.
[97]. “Developing a global vaccine with the help of a digital twin,” Meta, retrieved on January 7, 2025, https://forwork.meta.com/case-studies/how-vr-tech-boosted-pfizers-covid-response/.
[98]. “Beating the Pandemic in Virtual Reality,” Nanome, November 21, 2022, https://nanome.ai/blog/beating-the-pandemic-in-virtual-reality/; Jennifer Kite-Powell, “See How Virtual Reality Is Helping Scientists Collaborate On Drug Design And Discovery,” Forbes, May 21, 2021, https://www.forbes.com/sites/jenniferhicks/2021/05/21/see-how-virtual-reality-is-helping-scientists-collaborate-on-drug-design-and-discovery/.
[99]. Gail Dutton, “Extended Reality Helps Drug Designers Realize Bold Visons,” Genetic Engineering and Biotechnology News, March 1, 2024, https://www.genengnews.com/topics/artificial-intelligence/extended-reality-helps-drug-designers-realize-bold-visions/.
[100]. “Press,” Nanome, accessed on January 10, 2025, https://nanome.ai/press.
[101]. Ibid.
[102]. Patrick Liu, “How Augmented Reality Will Transform the Fitness Industry,” TechCrunch, https://techcrunch.com/sponsor/photonlens/how-augmented-reality-will-transform-the-fitness-industry/
[103]. “Best-selling Nintendo Wii game titles worldwide as of September 2024,” Statista, November 2024, https://www.statista.com/statistics/248204/top-selling-nintendo-wii-titles-worldwide/.
[104]. Liu, “How Augmented Reality Will Transform the Fitness Industry.”
[105]. Will Mitchell, “Hit your 2024 exercise goals with these VR fitness apps and games,” NPR, January 17, 2024, https://www.npr.org/2024/01/17/1223996232/2024-best-vr-fitness-apps-and-games.
[106]. Lynne M. Taylor et al., “Active Video Games for Improving Physical Performance Measures in Older People: A Meta-analysis,” Journal of Geriatric Physical Therapy, March 2016, https://pmc.ncbi.nlm.nih.gov/articles/PMC5895114/.
[107]. FitXR, accessed on April 15, 2025, https://fitxr.com/.
[108]. “Physical activity,” World Health Organization, June 26, 2024, https://www.who.int/news-room/fact-sheets/detail/physical-activity.
[109]. FitXR.
[110]. Ibid.
[111]. Sharon L. Farra, “Comparative Cost of Virtual Reality Training and Live Exercises for Training Hospital Workers for Evacuation,” Computers, Informatics, Nursing, Vol. 37 (September 2019), https://journals.lww.com/cinjournal/abstract/2019/09000/comparative_cost_of_virtual_reality_training_and.3.aspx.
[112]. “America’s Hospitals and Health Systems Continue to Face Escalating Operational Costs and Economic Pressures as They Care for Patients and Communities,” American Hospital Association, May 2024, https://www.aha.org/costsofcaring.
[113]. “Health Workers Face a Mental Health Crisis,” Center for Disease Control, October 24, 2023, https://www.cdc.gov/vitalsigns/health-worker-mental-health/index.html.
[114]. “How health systems and educators can work to close the talent gap,” McKinsey, September 29, 2023, https://www.mckinsey.com/industries/healthcare/our-insights/how-health-systems-and-educators-can-work-to-close-the-talent-gap.
[115]. Ibid.
[116]. Ibid.
[117]. “State of the U.S. Health Care Workforce, 2024,” National Center for Health Workforce Analysis, November 2024, https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/state-of-the-health-workforce-report-2024.pdf.
[118]. Ibid.
[119]. “Virtual Rehab Experiential Care”, U.S. Department of Veterans Affairs, July 2024, https://marketplace.va.gov/innovations/virtual-rehab-experiential-care.
[120]. “XR Association Developer’s Guide: Chapter 5, Designing Immersive Solutions for Healthcare,” XR Association, December 2023.
[121]. “Navigating the FDA Regulatory Landscape,” XR Association, accessed on December 16, 2024, https://xra.org/wp-content/uploads/2024/11/Navigating-the-FDA-Regulatory-Landscape.pdf.
[122]. “Augmented Reality and Virtual Reality in Medical Devices,” Food and Drug Administration, September 6, 2024, https://www.fda.gov/medical-devices/digital-health-center-excellence/augmented-reality-and-virtual-reality-medical-devices.
[123]. “Navigating the FDA Regulatory Landscape,” XR Association.
[124]. “How to Find and Effectively Use Predicate Devices,” Food and Drug Administration, September 4, 2018, https://www.fda.gov/medical-devices/premarket-notification-510k/how-find-and-effectively-use-predicate-devices.
[125]. “Navigating the FDA Regulatory Landscape,” XR Association.
[126]. Ibid.
[127]. “Navigating the FDA Regulatory Landscape,” XR Association.
[128]. Ryan Beams et al., “Evaluation Challenges for the Application of Extended Reality Devices in Medicine,” Journal of Digital Imaging (November 2021), https://link.springer.com/article/10.1007/s10278-022-00622-x.
[129]. “XR Association Developer’s Guide: Chapter 5, Designing Immersive Solutions for Healthcare,” XR Association, December 2023.
[130]. “MediView transforms medical imaging with mixed reality using Microsoft HoloLens 2, bringing advanced procedures to more patients,” Microsoft, November 21, 2023, https://www.microsoft.com/en/customers/story/1705331318505418671-mediview-hololens-health-provider-en-united-states.
[131]. Beams et al., “Evaluation Challenges for the Application of Extended Reality Devices in Medicine.”
[132]. Alex Ambrose, “Comments Before NIST Regarding Preliminary Research on Cybersecurity and Privacy Standards for Immersive Technologies” (ITIF, July 26, 2024), https://itif.org/publications/2024/07/26/comments-before-nist-regarding-research-cybersecurity-privacy-standards-immersive-technologies/.
[133]. Ellysse Dick, “Balancing User Privacy and Innovation in Augmented and Virtual Reality” (ITIF, March 4, 2021), https://itif.org/publications/2021/03/04/balancing-user-privacy-and-innovation-augmented-and-virtual-reality/.
[134]. “Children’s Online Privacy Protection Rule (“COPPA”),” Federal Trade Commission, accessed on May 9, 2025, https://www.ftc.gov/legal-library/browse/rules/childrens-online-privacy-protection-rule-coppa.
[135]. “FERPA,” U.S. Department of Education, accessed on May 9, 2025, https://studentprivacy.ed.gov/ferpa.
[136]. “Summary of the HIPAA Privacy Rule,” Department of Health and Human Services, accessed on May 9, 2025, https://www.hhs.gov/hipaa/for-professionals/privacy/laws-regulations/index.html.
[137]. “Health Insurance Portability and Accountability Act of 1996 (HIPAA),” Centers for Disease Control, September 10, 2024, https://www.cdc.gov/phlp/php/resources/health-insurance-portability-and-accountability-act-of-1996-hipaa.html.
[138]. Jenna McLaughlin, “Cyberattacks on hospitals ‘should be considered a regional disaster,’ researchers find,” NPR, June 25, 2023, https://www.npr.org/2023/06/25/1184025963/cyberattacks-hospitals-ransomware.
[139]. Vibhu Mishra, “Cyberattacks on healthcare: A global threat that can’t be ignored,” United Nations, November 8, 2024, https://news.un.org/en/story/2024/11/1156751.
[140]. Ambrose, “Comments Before NIST Regarding Preliminary Research on Cybersecurity and Privacy Standards for Immersive Technologies.”
[141]. Claire Hughes, “Overcoming Cybersickness in Virtual and Augmented Reality,” VR/AR Association, February 23, 2021, https://www.thevrara.com/blog2/2021/2/23/overcoming-cybersickness-in-virtual-and-augmented-reality-dinteract-cyber.
[142]. Ambrose, “User Safety in AR/VR: Protecting Kids.”
[143]. Ibid.
[144]. Dick, “Balancing User Privacy and Innovation in Augmented and Virtual Reality.”
[145]. “Overview,” National Institutes of Health, accessed on May 7, 2025, https://braininitiative.nih.gov/about/overview.
[146]. “Understanding the BRAIN Initiative Budget,” National Institutes of Health, accessed on May 7, 2025, https://braininitiative.nih.gov/funding/understanding-brain-initiative-budget.
[147]. “Our Mission,” Center for Medical Innovation in Extended Reality, retrieved on October 3, 2024, https://www.mixrcenter.org/.
[148]. Barbosu, “Harnessing AI to Accelerate Innovation in the Biopharmaceutical Industry.”
[149]. Ibid.
[150]. “Health Workforce Programs,” Health Resources and Services Administration, accessed on May 15, 2025, https://bhw.hrsa.gov/programs.
[151]. “Training,” U.S. Department of Labor, accessed on May 15, 2025, https://www.dol.gov/general/topic/training.
[152]. Ravi Shankar et al., “Virtual reality for stress management and burnout reduction in nursing: A systematic review protocol,” PLoS One, April 7, 2025, https://pubmed.ncbi.nlm.nih.gov/40193343/.
[153]. “How health systems and educators can work to close the talent gap,” McKinsey, September 29, 2023, https://www.mckinsey.com/industries/healthcare/our-insights/how-health-systems-and-educators-can-work-to-close-the-talent-gap; “2023 Annual Report,” Food and Drug Administration, 2023, https://www.fda.gov/media/175479/download?attachment.
[154]. “Breakthrough Devices Program,” Food and Drug Administration, November 7, 2024, https://www.fda.gov/medical-devices/how-study-and-market-your-device/breakthrough-devices-program#s1.
[155]. “Safer Technologies Program for Medical Devices,” Food and Drug Administration, March 15, 2021, https://www.fda.gov/medical-devices/how-study-and-market-your-device/safer-technologies-program-step-medical-devices#what.
[156]. “2023 Annual Report,” Food and Drug Administration; “Navigating the FDA Regulatory Landscape,” XR Association; Juan Londoño, “The FDA Is Unprepared for Tech-Driven Innovations,” DC Journal, March 15, 2025, https://dcjournal.com/the-fda-is-unprepared-for-tech-driven-innovations/.
[157]. Nick Paul Taylor, “FDA breakthrough device decisions rebound after recent declines,” MedTechDive, November 14, 2024, https://www.medtechdive.com/news/fda-breakthrough-devices-2024-pi-cardia-renata-neuros/732485/.
[158]. “National Evaluation System for health Technology (NEST)”, Food and Drug Administration, retrieved on March 6, 2025, https://www.fda.gov/about-fda/cdrh-reports/national-evaluation-system-health-technology-nest; “Our Work,” Medical Device Innovation Consortium, retrieved on March 6, 2025, https://mdic.org/our-work/; “About Us,” National Evaluation System for Health Technology, retrieved on March 6, 2025, https://nestcc.org/about/about-us/.
[159]. “Healthcare Common Procedure Coding System,” Center for Medicare and Medicaid Services, retrieved on January 7, 2025, https://www.cms.gov/medicare/coding-billing/healthcare-common-procedure-system.
[160]. Frank Diamond, “CMS ruling paves way for virtual reality companies to obtain reimbursement from payers,” Fierce Healthcare, March 21, 2023, https://www.fiercehealthcare.com/payers/cms-ruling-paves-way-virtual-reality-companies-obtain-reimbursement-payers
[161]. Diamond, “CMS ruling paves way for virtual reality companies to obtain reimbursement from payers,”; Anastassia Gliadkovskaya, “2024 Outlook: Despite hurdles, stakeholders bullish on VR in behavioral health,” Fierce Healthcare, December 28, 2023, https://www.fiercehealthcare.com/health-tech/2024-outlook-despite-hurdles-stakeholders-bullish-virtual-reality.
[162]. Peter J. Neumann et al., “Medicare’s new transitional coverage of emerging technologies program doesn’t go far enough,” Statnews, August 28, 2024, https://www.statnews.com/2024/08/28/medicare-ced-tcet-coverage-emerging-technologies-devices/.
[163]. John Walker, “New Solution, Same Problem,” American Action Forum, September 6, 2024, https://www.americanactionforum.org/weekly-checkup/new-solution-same-problem/.
[164]. Neumann et al., “Medicare’s new transitional coverage of emerging technologies program doesn’t go far enough.”
[165]. Walker, “New Solution, Same Problem.”
[166]. “Final Notice—Transitional Coverage for Emerging Technologies (CMS-3421-FN),” Centers for Medicare and Medicaid Services, August 7, 2024, https://www.cms.gov/newsroom/fact-sheets/final-notice-transitional-coverage-emerging-technologies-cms-3421-fn.
[167]. Walker, “New Solution, Same Problem.”
[168]. Neumann et al., “Medicare’s new transitional coverage of emerging technologies program doesn’t go far enough.”
[169]. Bobby McMillin, Monique Nolan, and Dorothy Isgur, “Congress Responds to the Proposed Transitional Coverage for Emerging Technologies Medicare Pathway,” Arnold and Porter, August 2, 2023, https://www.arnoldporter.com/en/perspectives/advisories/2023/08/congress-responds-to-tcet.
[170]. Susan Milligan, “Congress Faces March 31 Deadline to Extend Medicare Telehealth Coverage,” AARP, February 27, 2025, https://www.aarp.org/health/medicare-insurance/info-2025/medicare-telehealth-coverage-deadline.html.
[171]. Beams et al., “Evaluation Challenges for the Application of Extended Reality Devices in Medicine.”
[172]. Ibid.
[173]. “International Virtual Reality and Healthcare Association Web Site Launches with 40 Founding Member Organizations,” IVHRA, May 7, 2019, https://ivrha.org/international-virtual-reality-and-healthcare-association-ivrha-web-site-launches-with-40-founding-member-organizations/.
[174]. Frank Konkel, “VA’s Extended Reality Network Expanding Across Agency,” Nextgov, August 17, 2021, https://www.nextgov.com/emerging-tech/2021/08/vas-extended-reality-network-expanding-across-agency/184598/; Anne Bailey, “VA expands virtual reality for Veteran rehabilitation,” U.S. Department of Veterans Affairs, April 3, 2023, https://news.va.gov/117227/va-expands-virtual-reality-rehabilitation/.
[175]. “XR Association Endorses the House Reality Caucus Appropriations Request for FY26,” XR Association, April 29, 2025, https://xra.org/xr-association-endorses-the-house-reality-caucus-appropriations-request-for-fy26/.
[176]. “Augmented Reality and Virtual Reality Medical Devices: Questions to Consider,” Food and Drug Administration, accessed on December 12, 2024, https://www.fda.gov/medical-devices/digital-health-center-excellence/augmented-reality-and-virtual-reality-medical-devices-questions-consider.
[177]. Sophie Brassel et al., “Speech-Language Pathologists’ Views of Using Virtual Reality for Managing Cognitive-Communication Disorders Following Traumatic Brain Injury,” American Speech-Language-Hearing Association, September 8, 2022, https://pubmed.ncbi.nlm.nih.gov/36580534/.
Editors’ Recommendations
Related
November 18, 2020
ITIF Technology Explainer: What Is AR/VR?
August 29, 2024

